- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Click to find the locations nearest youFind locations by region
See all locations -
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Mental Health Town Hall
Tuesday, April 23, 2024Join Children’s Hospital Colorado pediatric experts for a virtual...
-
Research & Innovation
- Overview
- Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.



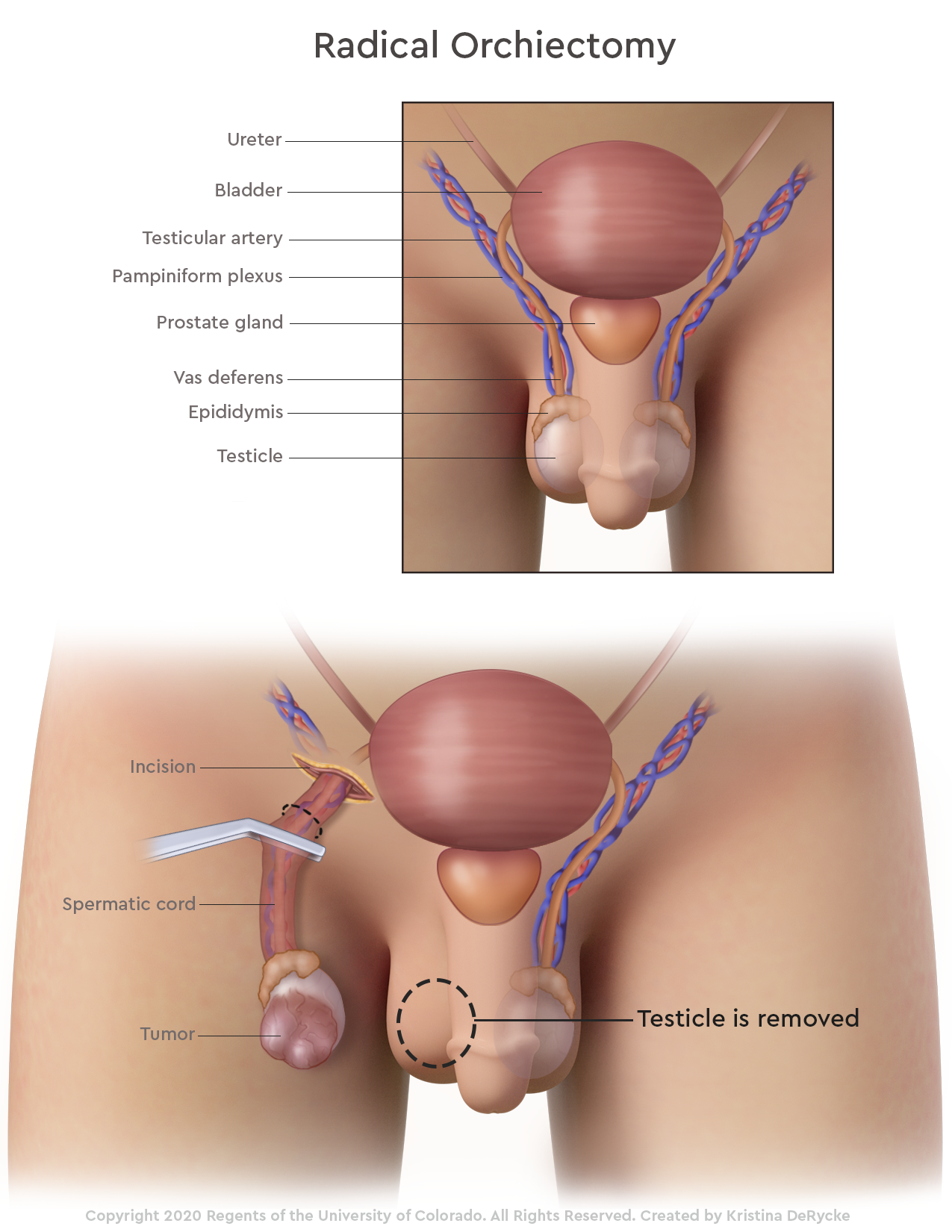
An orchiectomy is the surgical removal of a testicle. While doctors can perform imaging tests such as an ultrasound as a first step in the diagnosis of a testicular mass, the final diagnosis cannot be confirmed until an orchiectomy is performed. Testicular masses are commonly found to be testicular cancer. There are two types of orchiectomies – a radical orchiectomy and a partial orchiectomy.
What is a radical orchiectomy?
A radical orchiectomy is the complete removal of the testicle that includes the testicular mass. This is the most common operation performed for testicular cancer worldwide.
What is a partial orchiectomy?
A partial orchiectomy removes the part of the testicle that has the mass, while leaving the other “normal” part of the testicle in place. As our understanding of testicular cancer and surgical techniques have improved over time, a partial orchiectomy has become an option for some patients. A partial orchiectomy removes part of the testicle in an effort to spare as much of the testicle as possible.

Why might a doctor recommend a radical orchiectomy or partial orchiectomy?
A radical orchiectomy involves removing the testicle and spermatic cord, which is where the testicle descends when the boy is developing as a fetus. As a male fetus develops, the testes develop near where the kidneys are developing in the fetus. As the fetus grows, at about the eighth month of pregnancy, the testicles descend from the abdomen into the scrotum. This is why premature infants have a higher likelihood of having undescended testicles.
The blood supply, lymphatic drainage and nerves to the testicle originate near the kidney on the side the testicles descend. Once these structures descend, they fuse with muscles of the body wall to form the spermatic cord. To correctly stage and prevent any cancer from spreading, the spermatic cord must be removed as high as possible, which is why the incision for a radical orchiectomy is made in the groin rather than the scrotum.
For those whose cancer has spread from the testicle to elsewhere in the body or to the lymph nodes, a radical orchiectomy is an important first step in the diagnosis and management of disease. Knowing the type of cancer may help guide chemotherapy or radiation treatments.
What to expect during an orchiectomy
Radical orchiectomy
Your son’s surgeon performs the surgery under general anesthesia. The surgeon will make a 5- to 8-centimeter incision in the groin, which gives the surgeon access to both the testicle and the spermatic cord. The surgeon will carefully remove the testicle and the spermatic cord and close the incisions.
Partial orchiectomy
In the case of a partial orchiectomy, the initial steps are similar to the radical orchiectomy. However, instead of removing the entire testicle, we remove just the tumor and send it to a pathologist for examination. If there is an indication that the whole testicle needs to be removed based on the type of tumor they see, we will do so at that time. If we determine a partial orchiectomy is adequate, we will place the remaining testicle back into the scrotum and complete the surgery.
Possible complications of an orchiectomy
The biggest risk of an orchiectomy is hematoma, or bleeding into the scrotum. It is very common for the scrotum to be bruised, swollen and tender for 2 to 4 weeks after surgery. However, a large, purple-appearing scrotum can indicate a hematoma. We can prevent hematoma with a compressive dressing, tight-fitting undergarments and ice packs.
Nerve injury can occur if the nerve is damaged during dissection. This is more common in those who have undergone prior surgery (usually for an undescended testicle or hernia repair). Your child may have decreased sensation in their thigh, scrotum or base of the penis. It is often temporary but can take several weeks or months to improve. An inguinal hernia can also occur if the incision is not closed properly or if the closure breaks down.
If you have any questions or concerns after the procedure, call the ParentSmart Healthline at 1-855-KID-INFO (543-4636). Caring pediatric nurses are available 24 hours a day, 7 days a week to help answer your questions.
What to expect after an orchiectomy
If none of the complications above occur, we usually recommend that patients minimize strenuous activities for 2 to 4 weeks afterwards, which will help to prevent the development of a hernia. Your child’s doctor will schedule a follow-up visit to ensure they minimize any risk of complications. Because many orchiectomies are performed because of testicular cancer, your child’s doctor will continue to schedule follow-up visits based on the plan of cancer treatment they have developed.
Why choose us for an orchiectomy?
Children’s Hospital Colorado houses a surgical oncology team that includes a urology surgeon. These surgeons specialize specifically in the surgical treatment of urologic cancer. Our teams work together closely to ensure an optimal outcome. Using their expertise and state-of-the-art equipment, the surgical team strives to removal all remnants of the cancer while leaving as much of the healthy tissue and organs intact. In past decades, a surgeon may have preferred to perform a radical orchiectomy to ensure all the cancerous tissue is removed. Now, after having performed many of these procedures and using advanced technology, we are now able to perform surgeries with much more precision and partial orchiectomies are possible in select patients.



 720-777-0123
720-777-0123




 At Children’s Hospital Colorado, we treat the big things, the small things and everything in between.
At Children’s Hospital Colorado, we treat the big things, the small things and everything in between.