Could the complement immune system be responsible for pulmonary hypertension?
Most patients don’t feel symptoms until it’s too late: Widespread, potentially irreversible changes to the entire cardiopulmonary system are already well underway. Some patients respond well to treatment. Others rapidly decline. There is no cure. With nearly $14 million in funding from the National Institutes of Health, a large team of researchers is investigating a potential root culprit: the destructive potential of the innate immune system.
The many triggers of pulmonary hypertension
At first glance, pulmonary hypertension looks pretty simple. It’s an increase in blood pressure in the lungs.
A lot of things can trigger it. Genetics, infection, drugs, tumors, metabolic dysfunction. It’s a complication of disease. It can occur idiopathically. It affects all ages, from newborns to the very old. It takes many forms.
But the mechanics are the same: some insult causes the pulmonary artery to constrict. The subsequent rise in pressure damages the vessels and hampers gas exchange, leading to hypoxia, which further damages the artery. Those insults trigger inflammation, and that’s where things seem to go awry.
Inflammation stiffens and thickens the artery, ramping up the pressure, creating an environment so hostile and diseased it warps cells’ genetic expression at the molecular level. It doesn’t just affect the cardiopulmonary system. It seems to fundamentally rebuild the system. Often, the changes are irreversible.
Theoretically, you should be able to reverse the process, or at least to stop it from progressing, by relaxing the pulmonary artery. Indeed, dozens of vasodilators have been tried, and some of them, in some situations, can slow the cycle down.
Just as often, though, they don’t. And when they don’t, there’s not much else.
Tracing the origins
In many ways, pulmonary hypertension, or PH, is still poorly understood. Still, few people in the world can claim to have done as much to understand it as pediatric critical care specialist Kurt Stenmark, MD. His work has been supported for 45 years by the longest continuously funded program project grant in the Division of Lung Diseases of the NIH. He helped found and has led the Division of Critical Care at Children’s Hospital Colorado since 1987. He’s led the Cardiovascular Pulmonary Research Lab at the neighboring University of Colorado School of Medicine — the CVP for short — since 2005, growing a team of more than 30 of the world’s foremost pulmonary hypertension researchers. He’s published more than 350 papers and contributed to hundreds more. Next year he’ll lead the Pulmonary Vascular Research Institute, a global research consortium, as the first pediatrician ever to serve as president.
Along with his close colleagues Maria Frid, PhD, a basic scientist specializing in vascular disease, and Rubin Tuder, MD, pathologist and Director of the Translational Lung Program at the University of Colorado School of Medicine, he’s been pursuing PH’s deepest question: How does it start?
The role of inflammation in pulmonary hypertension
A key driver seems to be inflammation. Drs. Stenmark, Tuder and team were the first to correlate the prevalence of pro-inflammatory mediators with thickening of the arterial wall. Inflammation drives epigenetic changes, which alter cells’ metabolism and changes their gene expression. Cells become resistant to death, as they do in cancer.
In fact, when the team looked at the cause of death in hundreds of blood and tissue samples from patients who’d died of PH, they found that inflammation was invariably involved. That insight led to a flurry of studies in the last decade investigating the role of cytokines in driving inflammation.
“Some of these cytokines are always present in PH, and the more they are, the worse patients do,” Dr. Stenmark says. “People have tried cytokine therapies to knock them out one by one. One tried IL6, another tried IL1, another tried TNF. People invested millions of dollars.”
He shrugs. “It didn’t really work out.”
Complement: a new hypothesis
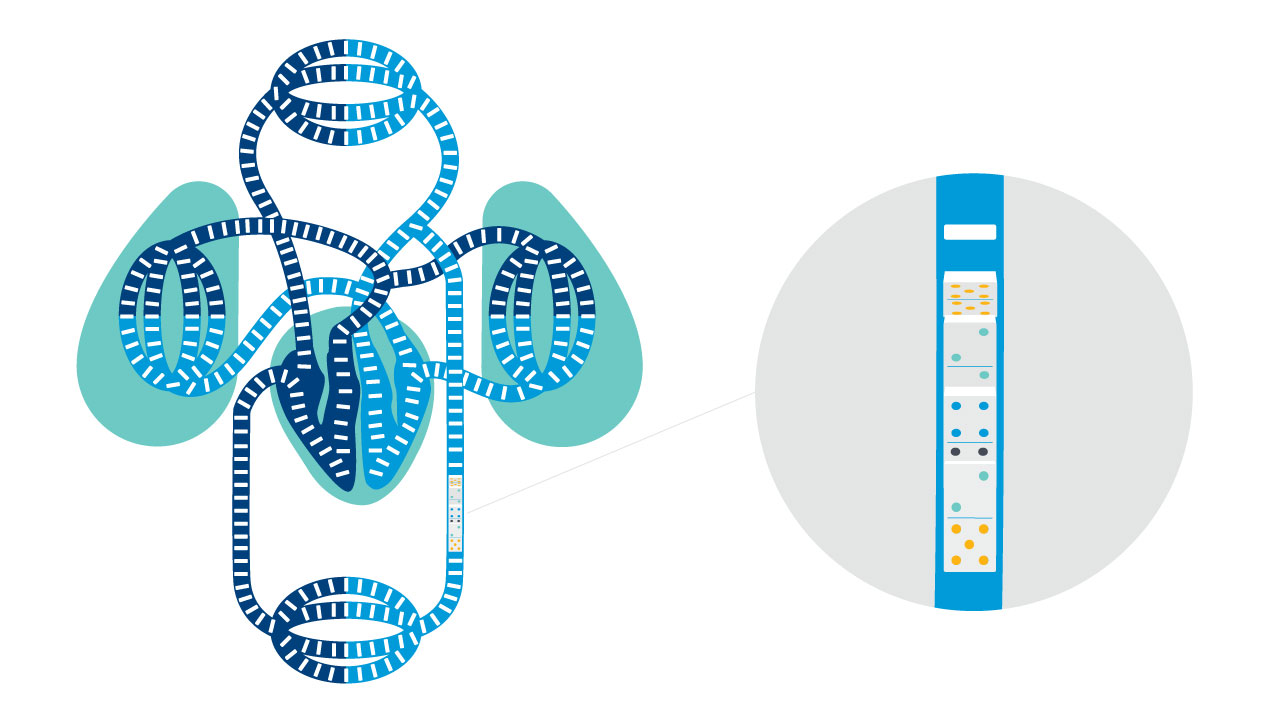
The complement immune system is one of the body’s first lines of defense. Innately programmed to destroy viruses, damaged cells and other pathogens, the 30-some proteins of the complement system form a cascade, knocking each other down like dominoes and recruiting killer cells and inflammatory compounds to the site of an insult.
Dr. Stenmark and his team knew inflammation drove the disease process. What they didn’t know was what was driving the inflammation. A study speculating on the potential role of complement in abdominal aortic aneurism, another large vessel disease, provided the lightbulb moment for Dr. Frid. Dr. Stenmark gave it the greenlight and they got to work.
They stained tissue samples. Complement showed up. They induced hypoxia in small animal models, comparing controls with models mutated to lack key complement proteins. The control models got PH. But some of the mutated ones didn’t.
The absence of those complement proteins, namely Cfb and C5, dramatically reduced the vascular inflammation and cytokine production. When they knocked out the antibody immunoglobulin G in small animal models, that also seemed to protect against vascular change.
Mapping the PH proteome
Using cutting-edge mass spectrometry techniques, molecular geneticist Kirk Hansen, PhD, analyzed every single protein expressed throughout the pulmonary vasculature in PH and control tissues, some 1,300 proteins altogether. It was the most detailed analysis of the pulmonary vascular proteome in PH to date. Complement components were some of the most altered proteins observed in PH tissues. The team worked with researchers at Harvard University and the Imperial College of London to identify 18 clinically relevant proteins altogether, heavily populated by complement intermediaries, that served as good markers of outcomes of disease.
Those discoveries have fundamentally altered the direction of the entire CVP, and the work is just beginning. Calculations are massive and difficult. Powerful computers crunch numbers day and night.
Four angles on PH and complement
Dr. Stenmark’s Program Project Grant funds four main projects centered around exploring the role of complement in pulmonary hypertension. The ultimate translational goal: identify biomarkers of inflammation, better define heterogeneity in disease progression and develop therapies to reduce pro-inflammatory signaling.
Immunoglobulin-driven activation of the complement cascade as a critical determinant of pulmonary arterial hypertension initiation and progression
Complement is a system of proteins, arranged like dominoes to tip when provoked. Drs. Frid and Stenmark’s team demonstrated for the first time that immunoglobulins are involved in activation of the cascade in hypoxic PH. The question is, what do those complement fragments do once set in motion? The first project studies hypoxic pulmonary hypertension leveraging technologies like high-definition MRI to evaluate where complement fragments end up and what they do there. They’ll also test the efficacy of TT32, a novel targeted complement inhibitor developed by rheumatologist and co-investigator Michael Holers, MD, who previously used it successfully to modulate arthritis in animal models.
Role of complement-driven pulmonary vascular inflammation in pulmonary hypertension
PI: Brian Graham, MD, Critical Care, University of California San Francisco
“Schistosomiasis always activates complement,” says Dr. Stenmark. “It’s how the body tries to get rid of infection. The question is, why is it that some schistosomiasis patients get PH? Why does complement turn destructive?” Using specimens collected at Stanford University and two sites in Brazil, Dr. Graham’s team will use mass cytometry to correlate blood complement levels with leukocyte signatures, comparing the activation mechanisms of hypoxic and schistosomiasis-triggered PH.
Evaluation of the dynamic reciprocity between cells and the vessel matrix in pulmonary hypertension
PI: Rubin Tuder, MD
During the search for cytokine therapies, researchers at Stanford University phenotyped thousands of PH patient samples, correlating patient outcomes to various inflammatory markers. “The hard work is done,” says Dr. Stenmark. “Now we’re going to see if we can make correlations about different types of inflammation and outcomes and identify subtypes of patients who might benefit from treatment.” Dr. Tuder and his team will do it by analyzing enormous masses of data to define every protein and microRNA strand present in PH lesions from hundreds of patients.
Complement-driven platelet activation of pulmonary vascular remodeling in pulmonary hypertension
PI: Cassidy Delaney, MD, Neonatology, Children’s Colorado
“We know platelets and clotting factor into PH, but their role in remodeling and relationship to complement is unclear,” says Dr. Stenmark. “That’s a new area for research, but what’s also important is that the NIH is taking a risk on integrating a new clinician scientist.” The grant’s sole junior investigator, Dr. Delaney is studying endothelial cells’ increased expression of proteins that promote adhesion of platelets to the endothelia, whether that action is driven by complement, and what role those platelets play in recruiting inflammatory cells and compounds.
Complement, PH and COVID-19
“A lot of people who come in with COVID-19 are severely hypoxic,” Dr. Stenmark says. “We’re seeing evidence of vascular involvement, severe endothelial injury and cell death, inflammation, thrombosis. A lot of the same stuff we see in PH.”
In fact, endothelial cells play a key role in activating complement; Dr. Stenmark and team wondered if the SARS-CoV-2 virus, in conjunction with hypoxia, might be acting on endothelial cells to detonate complement, and whether anti-complement therapies aimed at the pulmonary-vascular endothelium might help. They’re now studying just that, with help from a $200,000 grant from the American Lung Association.
And those are just a few of the many, many projects the team is working on to understand the deep mechanisms of PH. Through two grants funded by the Department of Defense, for example, molecular biologists Hui Zhang, MD, and Cheng-Jun Hu, PhD, are now studying intracellular complement signaling contributing to inflammatory and metabolic processes that change the genetics of cells themselves. Someday, they hope, they may be able to use epigenetic modifiers to return the chromatin structure of cells distorted by PH to normal.
That day may still be a long way off.
“Medicine is hard,” says Dr. Stenmark. “People want medicine to take care of the problem and then it goes away. I wish it were that easy. We’re not under any pretenses that we’re going to cure pulmonary hypertension in the next five years.
“But,” he adds, “we are going to know a lot more about the role of complement.”
Featured Researchers
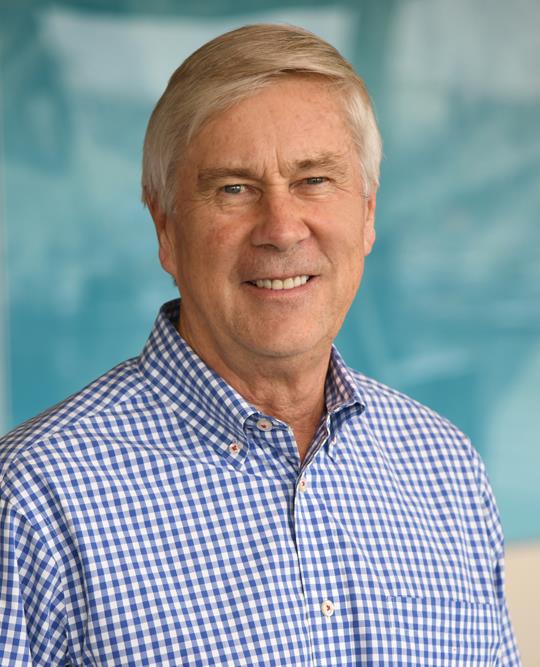
Kurt Stenmark, MD
Chair, Pediatric Critical Care Medicine
Pediatric Intensive Care Unit (PICU)
Children's Hospital Colorado
Professor
Pediatrics-Critical Care Medicine
University of Colorado School of Medicine
Maria Frid, PhD
Basic scientist specializing in vascular disease
University of Colorado School of Medicine

Rubin Tuder, MD
Professor
Medicine-Pulmonary Sciences and Critical Care
University of Colorado School of Medicine

Cassidy Delaney, MD
Neonatologist
Neonatal Intensive Care Unit
Children’s Hospital Colorado
Associate professor
Pediatrics-Neonatology
University of Colorado School of Medicine





 720-777-0123
720-777-0123