Key takeaways
-
False-positive rates for prenatal diagnosis of CoA often exceed 50% and accurate detection rates are less than 50%.
-
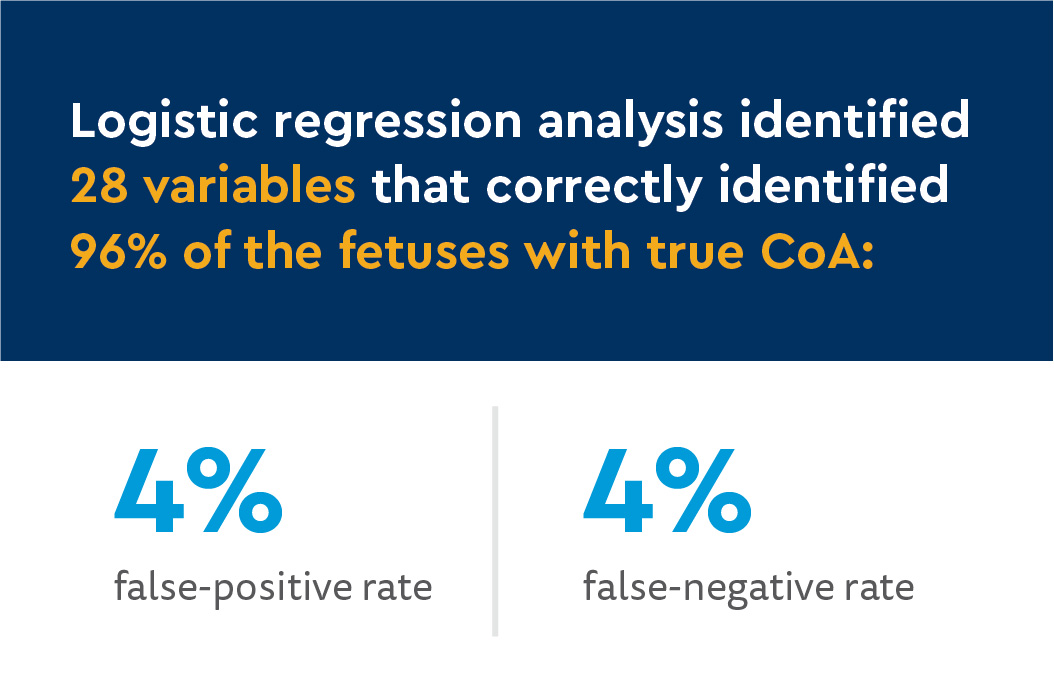
Study authors identified 28 variables which together separated true-positive from false-positive newborns with CoA.
-
Using these variables, researchers achieved 96% sensitivity and a 4% false-positive rate for CoA.
-
Use of these diagnostic tools could improve precision in identification of fetuses at risk for CoA.
Prenatal detection of coarctation of the aorta (CoA) improves postnatal outcomes and decreases morbidity and mortality.
When observing ventricle disproportion, a frequent first sign of CoA, false-positive rates often exceed 50%, and the accuracy of detection is less than 50%. Two-dimensional and pulsed Doppler measurements of the ventricles, mitral and tricuspid valves, aortic and pulmonary outflow tracts, aortic arch and isthmus have been used to improve detection with varying results.
When comparing fetuses with CoA confirmed postnatally compared to control fetuses in a previous study, researchers at the Colorado Fetal Care Center at Children’s Hospital Colorado found significant differences in:
- Epicardial size and shape in the four-chamber view (4CV)
- Size and shape of right ventricle (RV) and left ventricle (LV) chambers
- RV and LV global, longitudinal and transverse contractility
- LV stroke volume, cardiac output and ejection fraction
In this study, these variables were evaluated in fetuses suspected to have CoA. Researchers sought to determine which measurements of the 4CV and ventricles distinguished true positive CoA newborns from those with a prenatal diagnosis of CoA that was false-positive (FP-CoA).
Methods: prenatal and postnatal analysis of fetuses with suspected CoA
Fetal cardiology databases used:
- Children’s Hospital Colorado
- University of California, Los Angeles
Exclusions
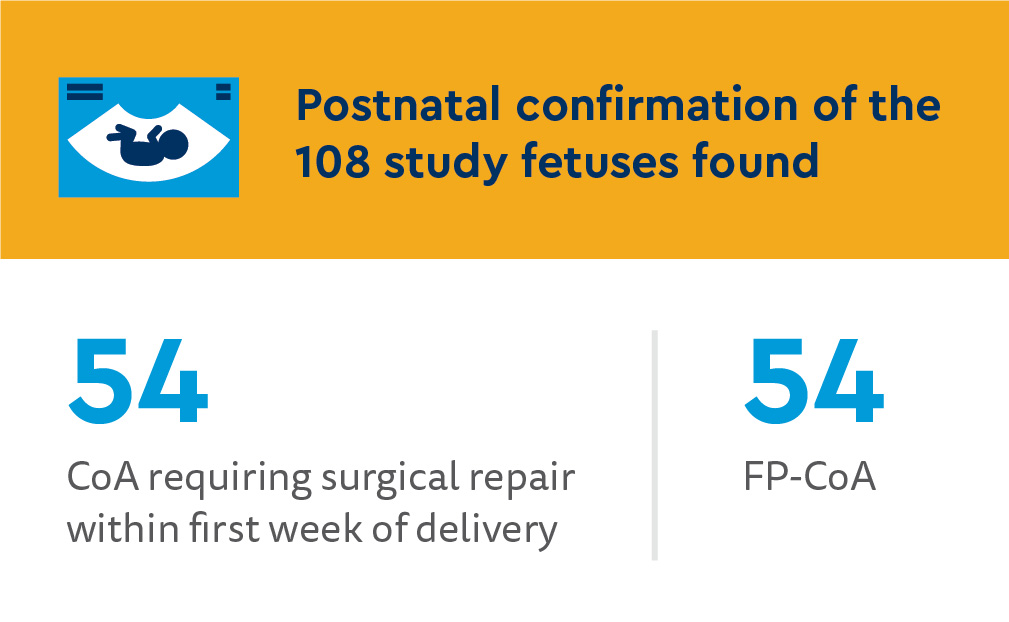
Digital Imaging and Communications in Medicine (DICOM) clips of the 4CV from the last examination prior to delivery were analyzed and classified as:
- Requiring postnatal surgery for CoA during the first week after delivery (true CoA)
- Postnatal FP-CoA
Epicardial shape and size measurements in 4CV during prenatal evaluation included:
- 4CV end-diastolic epicardial area
- Circumference
- Length
- Width
- Global sphericity index
Right and left ventricular endocardial measurements from speckle-tracking analysis from a single cardiac cycle determined:
- Ratio of end-diastolic areas
- Shape
- 24-segment sphericity index
- 24-segment transverse width
- Functional parameters
- Fractional area change
- Global longitudinal, free wall and septal strain
- Basal-apical-length basal free-wall, basal septal-wall fractional shortening
- Septal-wall annular plane systolic excursion
- 24-segment transverse-width fractional shortening
- LV end-diastolic and end-systolic volumes, stroke volume, cardiac output, ejection fraction
- RV/LV end-diastolic area ratio
Statistical analysis
- Mean and standard deviation of each cardiac value from 200 control fetuses used to compute Z-score for each measurement in each study fetus
- Logistic regression analysis on Z-score values identified variables separating true CoA group from FP-CoA group
Results: variables separating true CoA with false-positive CoA
Fetuses with true CoA had a significantly greater number of associated cardiac abnormalities (93% compared to 61% of FP-CoA).
Most common associated malformations
Variables included:
- Epicardial size in the 4CV
- Size and shape of RV and LV
- Abnormal contractility of RV and LV
The rate of RV/LV disproportion was not significantly different between the two groups (80% of true CoA, 76% of FP-CoA).
Discussion and conclusion: improved accuracy for predicting true CoA, need for postnatal surgery
There is a high degree of accuracy for the prediction of true CoA using speckle-tracking analysis of multiple measurements of size and shape on 4CV, ventricular size and shape, global and longitudinal contractility and LV ejection fraction in each fetus.
The study’s current approach is beneficial because the examiner obtains only end-systolic and end-diastolic measurements of RV and LV using speckle-tracking analysis and an end-diastolic image of the 4CV.
Use of these diagnostic tools could improve precision in identification of fetuses at risk for CoA. This is especially helpful when fetal position obstructs the aortic arch for imaging, which often occurs in the third trimester.
In conclusion, researchers identified 28 variables that separate true-positive from false-positive newborns with CoA with a sensitivity of 96% and a false-positive rate of 4%. By computing the probability of CoA, an examiner can evaluate a fetus with suspicion of CoA to determine the risk that the fetus will require surgery for CoA after birth.





 720-777-0123
720-777-0123










