Key takeaways
-
Fetal repair of MMC and myeloschisis in select cases leads to better outcomes for newborns with spinal bifida.
-
Colorado Fetal Care Center researchers reviewed nine years of patient data from surgical closure of MMC and myeloschisis.
-
They found a multilayered, watertight modified-myofascial closure leads to better outcomes.
Background: Fetal surgery reduces complications from myelomeningocele and myeloschisis
Spina bifida encompasses a wide range of neural tube defects, with the most serious and common being myelomeningocele (MMC). With MMC, the spinal cord extrudes into a cerebrospinal fluid-filled sac. When there is a defect but no cyst, the condition is known as myeloschisis. Neural tube defects increase the risk for spinal cord and peripheral nerve damage with subsequent postnatal complications.
Chiari II malformations are found in conjunction with MMC and myeloschisis and typically lead to postnatal hydrocephalus (HCP), a condition that results from an imbalance in cerebrospinal fluid drainage and commonly requires shunting.
Chiari II malformations include the following features:
- Hindbrain herniation (HBH) through the foramen magnum
- Brainstem abnormalities
- Low-lying venous sinuses
- Small posterior fossa
The Management of Myelomeningocele Study (MOMs) outlined the advantages of open fetal surgery for MMC and myeloschisis to reduce the need for HCP shunting. A watertight closure is believed to be necessary to improve HBH and reduce HCP. Surgical techniques for closing MMC and myeloschisis vary among surgeons and institutions.
In this study, led by neonatology and fetal medicine researchers at Children’s Hospital Colorado, researchers compared the results from two closure methods:
- Modified-myofascial closure: multilayer closure using raised myofascial flaps closed over the dura, followed by skin closure
- Non-myofascial closure: primary skin closure with or without a patch
Methods: comparing outcomes from modified-myofascial and primary skin closure
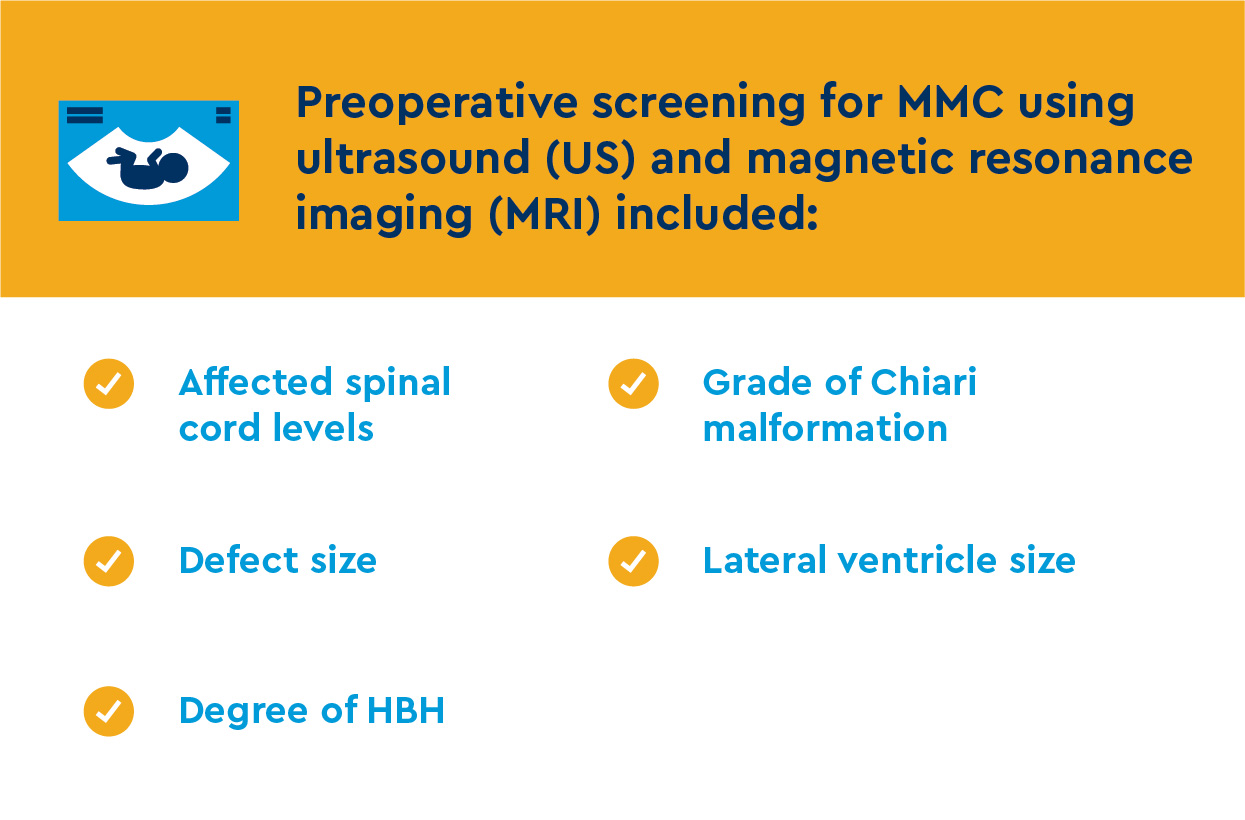
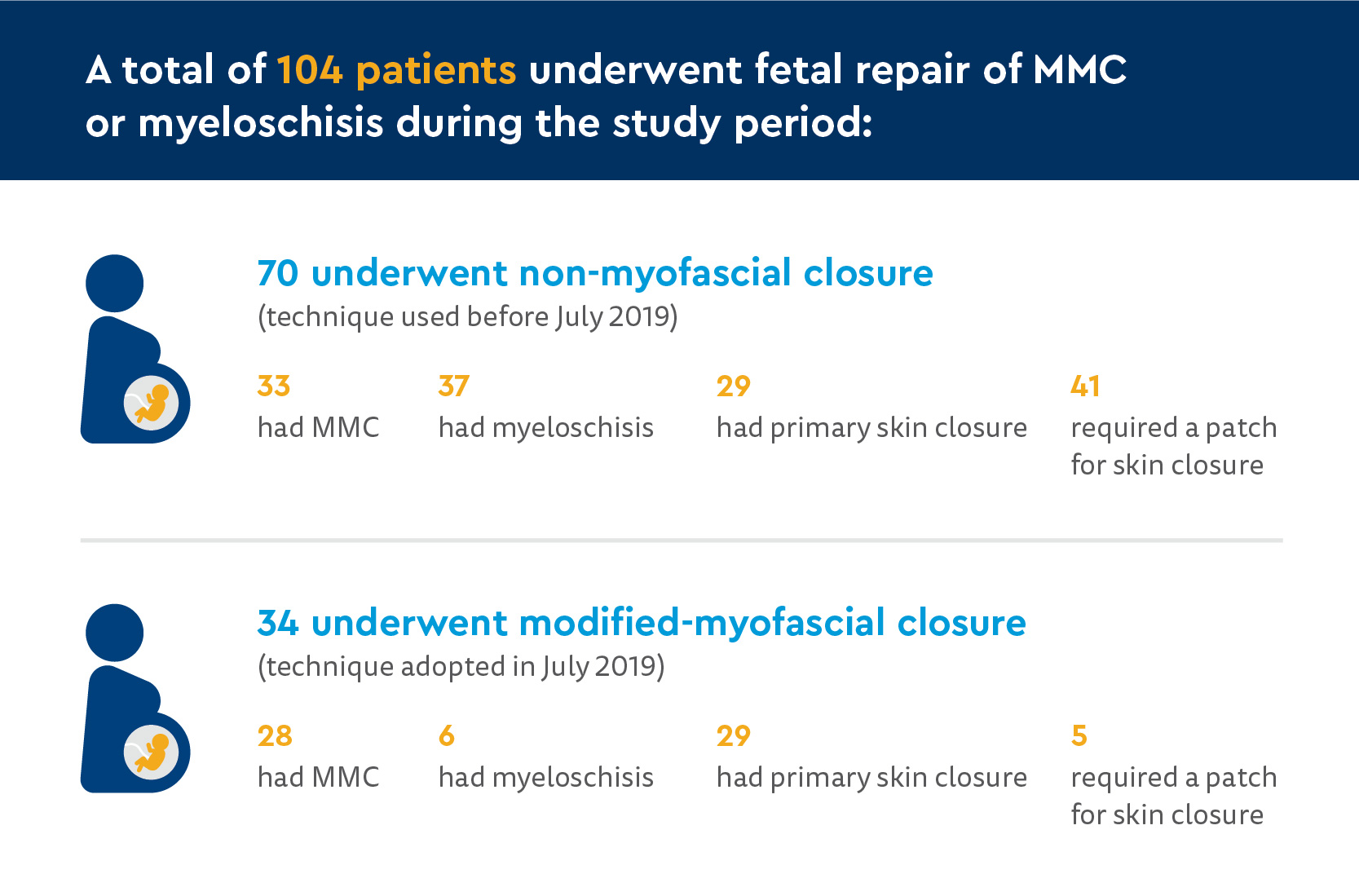
Researchers at the Colorado Fetal Care Center at Children’s Hospital Colorado conducted a retrospective comparative study using data from patients who underwent fetal repair of MMC or myeloschisis between March 2013 and February 2022. Before July 2019, non-myofascial closure was used. In July 2019 and thereafter, modified-myofascial closures were used.
After surgery, patients were closely monitored with serial ultrasounds.
Two weeks after discharge, patients had an ultrasound and MRI. Post-repair study data collected included:
- Lateral ventricle size
- Degree of HBH
- Change in HBH (degree of cerebellar descent relative to the foramen magnum)
Primary outcomes compared included:
- Improvement in HBH at two weeks post-discharge
- Need for surgical treatment for HCP by 12 months of age
Secondary outcomes compared included:
- Operative time
- Gestational age at time of delivery
- Age at time of HCP surgical treatment
Results: improved outcomes from modified-myofascial closure
Patient and pre-operative characteristics
There were no statistically significant differences between the two groups in:
- Surface area of the defect on either US or MRI
- Preoperative grade
- Preoperative lateral ventricle size
- Average gestational age at delivery
Operative findings
Among the two groups, there were statistically significant differences in:
- Operative time
- Modified-myofascial closure was longer
- Total procedure time was 137.2 minutes compared to 126.6 minutes
- Need for a patch
- 14.7% of modified-myofascial closures required a patch
- 58.6% of non-myofascial closures required a patch
- Improvement in HBH
- More improvement with primary skin closure
- More improvement with modified-myofascial closure
At 12-month follow-up (82 patients total):
- 62 were in non-myofascial repair group
- 26 patients (41.9%) required ventricular-peritoneal shunt (VPS) placement for hydrocephalus
- Median surgery age: 3.5 months old
- 20 were in modified-myofascial repair group
- Four patients (25%) required VPS placement for hydrocephalus
- One patient received choroid plexus cauterization in combination with endoscopic third ventriculostomy.
- Median surgery age: 8 months old
Discussion and conclusion: Modified-myofascial closure is the preferred method for treating MMC and myeloschisis
Comparing modified-myofascial closure with the non-myofascial closure for treating MMC and myeloschisis, Colorado Fetal Care Center researchers noted modified-myofascial closure resulted in:
- A decreased need for a patch placement
- Significantly increased improvement in HBH
- Potential to reduce the need for HCP surgical treatment
Stopping a cerebrospinal fluid (CSF) leak through a MMC or myeloschisis defect may prevent HBH by retaining a normal posterior fossa size. This makes watertight procedures a requirement for successful MMC or myeloschisis repair. Better HBH outcomes after primary skin repair versus patch repair support this premise.
This study provides evidence to support a modified-myofascial repair as the preferred surgical technique for MMC or myeloschisis. This technique provides multiple layers of soft-tissue closure to prevent CSF leaks, reduces the need for a skin patch and shows promise in reducing the need for HCP surgical treatment.





 720-777-0123
720-777-0123










