Key takeaways
-
In-utero repair of MMC typically requires the use of tocolytic agents like indomethacin, but it could cause the development of fetal DA.
-
When our researchers reviewed open fetal MMC repair cases, they found all fetuses experienced abnormal DA flow patterns and DA constriction during inhaled anesthesia.
-
Limiting the mother's exposure of indomethacin, providing less supplemental oxygen and using less inhaled anesthetics can help reduce frequency and/or severity of DA constriction and fetal cardiac dysfunction.
Research background
Fetuses who receive prenatal surgical repair of myelomeningocele (MMC) have improved neurological outcomes and a 50% reduction in ventriculoperitoneal shunting compared to those repaired after birth.
One of the risks after any fetal surgery is premature labor. Because of this risk, potent tocolytic agents (indomethacin, magnesium and nifedipine) are widely used before and after myelomeningocele (MMC) repair to prevent premature labor. Indomethacin can cause constriction of the fetal ductus arteriosus (DA), resulting in severe cardiac dysfunction.
While fetuses undergoing MMC repair are routinely exposed to indomethacin, a study of blood flow patterns in the fetal DA during the perioperative period hasn’t been performed. This preliminary study aimed to look at presence, timing and frequency of DA constriction before, during and after the repair.
Research methods
Pregnancies diagnosed with fetal MMC between January 2012 and July 2014 were reviewed from databases at the Colorado Institute for Maternal and Fetal Health. Fetal cardiologists and an anesthesiologist from the Colorado Fetal Care Center reviewed fetal echocardiograms and anesthesia records before, during and after MMC repair.
Prior to surgery, a dose of indomethacin (50mg orally) was given to the expectant mother at bedtime the evening prior to surgery and was followed at approximately 6 a.m. by a second dose (25mg).
In the OR, the expectant mother was monitored according to American Society of Anesthesia guidelines. The fetus was continually monitored in the operating room using echocardiography before, during and after the open MMC repair.
During the procedure, researchers sampled the DA using pulsed Doppler to obtain the peak, mean and end-diastolic velocities and calculated the DA Pulsatility Index (PI) as: (peak systolic velocity (PSV) – end-diastolic velocity (EDV)) / (time-averaged mean velocity (TAMV)).
For the first 48 hours after surgery, the magnesium infusion was continued and oral indomethacin (25 mg) was given every six hours, unless evidence of ductal constriction presented during surgery. In those cases, indomethacin was restarted only if uterine contractions occurred despite tocolysis with magnesium. Magnesium infusion was discontinued 48 hours after the repair and the expectant mother received nifedipine (20 mg) every six hours until delivery.
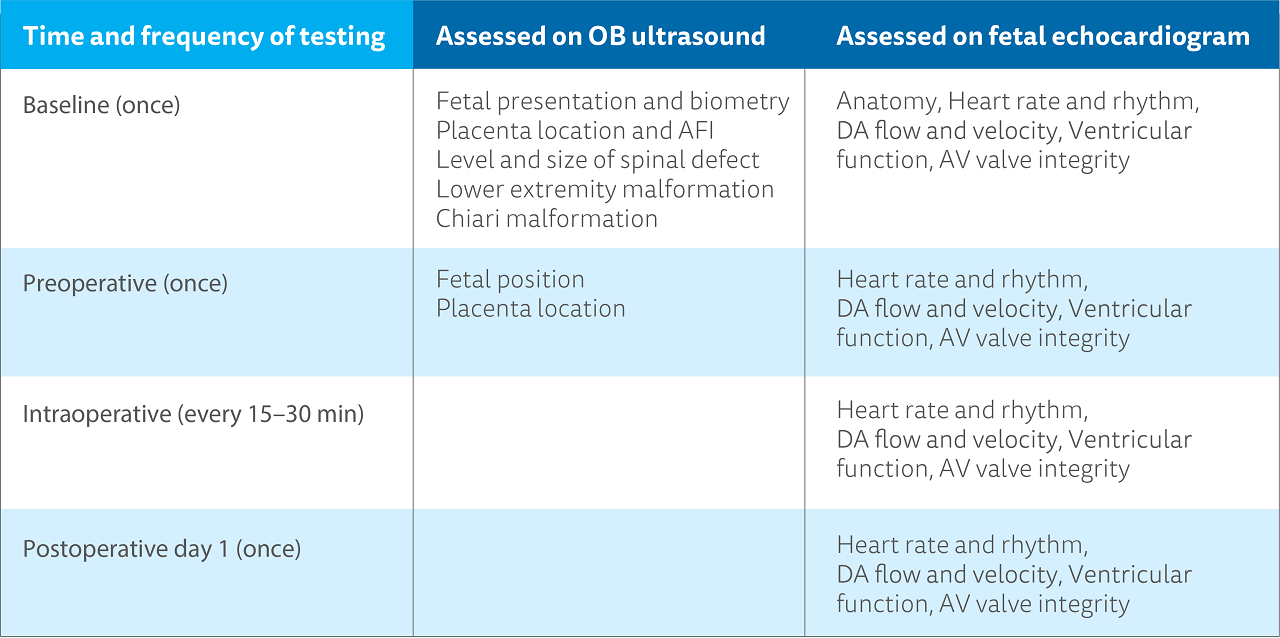
Fetal myelomeningocele repair evaluation timing and examination components
Research results
Of the 23 pregnancies referred to the Colorado Fetal Care Center for evaluation during the study period, 14 underwent open fetal MMC repair. Complete echocardiographic data were available in 10 pregnancies and these 10 comprise the study cohort.
Median gestational age of the cohort was 25 0/7 (23 3/7–25 5/7) weeks' gestation. At baseline, all fetuses had structurally normal hearts with normal biventricular and valve function and normal heart rates/rhythm. All fetuses survived the procedure and mothers were discharged on postoperative day four or five.
Researchers observed three distinct ductal flow patterns, characterizing the degree of ductal constriction. Two fetuses exhibited a severely constricted ductal flow pattern with concurrent moderate tricuspid insufficiency and right ventricular dysfunction during inhaled anesthesia.
In all fetuses, both the DA TAMV and EDV increased significantly between baseline and the time of inhaled anesthesia, consistent with DA constriction and this finding resolved by postoperative day two.
Research conclusion
The Colorado Fetal Care Center researchers observed abnormal DA flow patterns and DA constriction during inhaled anesthesia during open fetal MMC repair. Limiting maternal exposure to indomethacin, high levels of supplemental oxygen and decreasing the duration and concentration of inhaled anesthetic agents may reduce the incidence and/or severity of DA constriction and fetal cardiac dysfunction during open fetal surgery.





 720-777-0123
720-777-0123










