Key takeaways
-
Children’s Hospital Colorado researchers studied incidence of AKI, antenatal and postnatal predictors and impact of AKI on outcomes in infants with CDH.
-
They found AKI is common among infants with CDH and is associated with adverse outcomes.
-
Standardized care bundles to increase kidney function monitoring, limit nephrotoxin exposure and implement renal protective strategies could reduce AKI incidence and severity.
Research background: risk factors associated with adverse outcomes in neonates with congenital diaphragmatic hernia
A congenital diaphragmatic hernia (CDH) is a birth defect that can form between 8 to 10 weeks of gestation, occurring in one of every 3,000 live births. It compromises the in utero growth of and development of the heart and lungs, causing lung parenchyma and vascular abnormalities. In severe cases, about one-third of infants with CDH will require extracorporeal life support (ECLS). Compared to a 50 to 80% survival rate for neonates with isolated CHD, those requiring ECLS are approximately six times more likely to die.
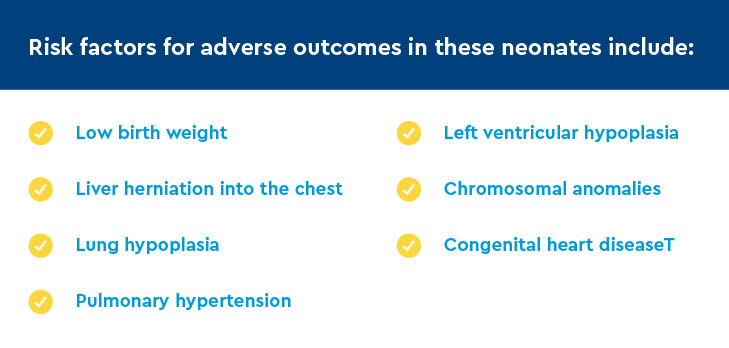
Acute kidney injury (AKI) is common in critically ill individuals, and neonates with CDH are at increased risk for both AKI and death. Yet, the risk factors responsible for development of AKI in infants with CDH are not known.
A multidisciplinary team of neonatology, pediatric nephrology and pediatric cardiology researchers at Children’s Colorado had three goals for this study of infants with CDH:
- Determine the incidence of AKI
- Examine antenatal characteristics and postnatal exposures associated with AKI
- Determine the impact of AKI on long-term outcomes, including length of stay, duration of mechanical ventilation and mortality
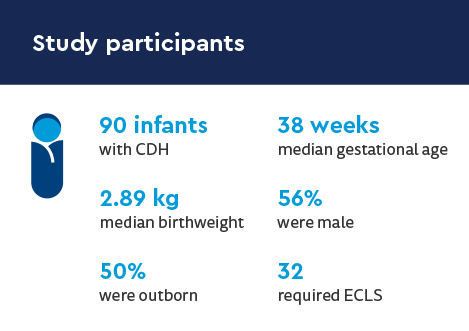
Research methods: a retrospective study of infants with CDH
The single-center retrospective study evaluated the electronic health records of infants with CDH managed in the neonatal intensive care unit (NICU) at Children’s Colorado between April 2009 and November 2017.
Extracted data included:
- Demographics
- Antenatal measures of CDH severity including presence or absence of liver herniation
- PPLV, TLV, LHR and O:E LHR from prenatal imaging for inborn patients
- Presence of CDH, congenital anomalies of the kidney and urinary tract, and chromosomal anomalies
- Day of initiation and duration of ECLS, if it was required
- Timing of CDH and abdominal closure surgery
- At Children’s Colorado, for patients requiring ECLS, CDH repair occurs in first 24 to 48 hours after ECLS cannulation
- Highest daily value of plasma free hemoglobin levels for patients on ECLS
- Daily net fluid balance
- To derive a fluid-corrected serum creatinine (SCr) calculation
AKI was defined and staged using the SCr criteria of the Neonatal Modified Kidney Disease Improving Global Outcomes definition.
Research results: incidence, severity outcomes for infants with CDH who develop acute kidney infection
Incidence of AKI
- 81% of infants requiring ECLS had AKI
- AKI occurred in 34 infants during first 30 days of life
- 44% were stage 1
- 29% were stage 2
- 27% were stage 3
- Day of life 12 was median day of diagnosis
- 9 had two episodes of AKI
- 2 had 3 episodes of AKI
- 8 required CRRT for metabolic control of uremia and fluid removal for anuria or oliguria
- All received ECLS
Antenatal and postnatal exposures associated with AKI
Infants with AKI were at higher risk for:
- lower antenatal assessments of fetal lung volume (mean PPLV 17.5%, median TLV 25 mL, median LHR 1, and median O: E LHR 38.5)
- liver herniation into the chest (85% occurrence)
- ECLS (95% occurrence, unadjusted)
Effects of AKI on long-term outcomes
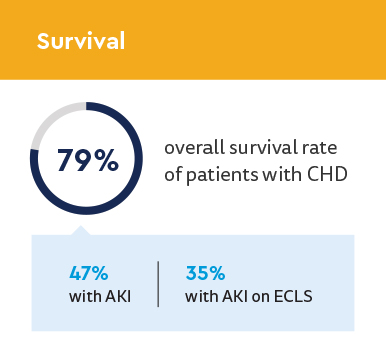
| Subgroup | Survival, n (%) |
|---|---|
| Entire Cohort, n=90 | 71 (78.8) |
| No AKI, n=56 | 55 (98.2) |
Any AKI, n=34
|
16 (47.1)*
|
| ECLS, n=32 | 15 (46.8) |
| ECLS and no AKI, n=6 | 6 (100) |
| ECLS and AKI, n=26 | 9 (34.6) |
- Mechanical ventilation: AKI associated with increased mechanical ventilation duration and length of stay
- 23.5 days median duration with AKI (13 days without)
- 59 days median length of stay with AKI (39 days without)
Research discussion and conclusion: AKI is common in infants CDH and associated with adverse outcomes
Key study findings
- AKI occurred in more than one-third of patients with CDH
- AKI associated with reduced survival
- Survival rates decreased with increasing stage of AKI
- ECLS greatest predictor for development of AKI
- Increased odds of AKI with ECLS exposure 72 and 24 hours prior to diagnosis of AKI and on the day of diagnosis
- Diuretic use, abdominal closure surgery, decrements in MAP and increased plasma free hemoglobin associated with increased odds of AK
Clinical considerations from study authors
- Infants with CDH requiring ECLS should undergo increased AKI surveillance and renal protective strategies since ECLS was the greatest risk factor for the development of AKI.
- Targeted AKI prevention strategies and increased AKI surveillance could improve mortality rates, especially in those requiring ECLS.
- Due to increased odds of AKI with abdominal closure surgery, silo placement in patients at risk for abdominal compartment syndrome should be contemplated.
- Following abdominal closure, study authors recommend close monitoring of intraabdominal pressure, utilizing bladder pressure as a surrogate, to mitigate the risk of AKI secondary to abdominal compartment syndrome
With limited therapies for treating established AKI, primary prevention of AKI is essential to improve outcomes. Standardized care bundles addressing AKI risk factors may reduce AKI incidence and severity.
Featured Researchers

Jason Gien, MD
Neonatologist
Neonatal Intensive Care Unit
Children's Hospital Colorado
Professor
Pediatrics-Neonatology
University of Colorado School of Medicine





 720-777-0123
720-777-0123










