Key takeaways
Three opportunities for the medical community to impact SUID rates:
-
Consistent data collection, reporting for all SUID cases
-
Engage families of preterm infants, infants with recent illness given their over-representation in SUID cases
-
Advocate for the ban of infant products marketed for use during infant sleep but are unsafe
Stats:
- 4,929 SUID cases reviewed in study
- 72% of all cases occurred with infants in unsafe sleep circumstances
- 75% of unsafe sleep deaths were linked to soft bedding
Research commentary background: an analysis of sudden unexpected infant death (SUID) data
In April 2021, the Centers for Disease Control and Prevention (CDC) published a study in Pediatrics that analyzed seven years of data from their Sudden Unexpected Infant Death (SUID) Case Registry.
SUID broadly defines the death of an infant under 1 year old that occurs under explained or unexplained circumstances, categorized by the following subgroups:
- Explained accidental suffocation - airway obstruction from overlay, soft bedding, or wedging or entrapment – considered preventable deaths
- Unexplained causes - sudden infant death syndrome (SIDS), unknown or undetermined causes
The study reviewed rates of SUID and identified associated demographic and medical factors. There were 4,929 SUID cases identified during the study period, which spanned from 2011-2017.
Mortality rates per 100,000 live births
- 97.3 overall SUID
- 79.6 unexpected SUID
Sunah Hwang, MD, MPH, PhD, a neonatologist at Children’s Hospital Colorado and Associate Professor of Pediatrics at the University of Colorado School of Medicine authored a commentary in the Pediatrics journal about the study’s findings. Dr. Hwang’s own research focuses on SUID/SIDS, safe infant sleep, disparities in maternal and infant health outcomes and transition from hospital to home for high-risk infants.
She identified three critical opportunities for the medical community to impact SUID rates:
- Consistent data collection and reporting for all SUID cases
- Engaging families of preterm infants and infants with recent illness given their over-representation in SUID cases
- Advocating for the ban of infant products that are marketed for use during infant sleep but are unsafe
Consistent data collection and reporting for SUID cases
SUID rates have not decreased for more than two decades, and almost 3,500 U.S. infants each year. SIDS and unintentional injuries are among the top causes of death in infants and newborns beyond 28 days of age. The rates are calculated by death certificate information but cause of death can be subjective and inconsistent.
In 2009, the CDC created the SUID Case Registry to supplement death certificate information and improve understanding of SUID. The population-based surveillance system is built on Child Death Review programs and uses data from multiple sources, including death certificates, scene investigations and autopsy reports.
The registry includes a standardized classification system and algorithm to better categorize and monitor SUID and its subgroups. Currently, only 18 states and jurisdictions, representing 30% of all SUID cases in the U.S, participate in the registry.

Study population
Compared to all SUID cases in the U.S., the registry is composed of more non-Hispanic Black (37% vs 30%) and fewer non- Hispanic white (42% vs 47%) infants. SUIDs occur in non-Hispanic Black and American Indian or Alaskan native infants approximately twice as often compared to the rate of SUIDs in the overall U.S. population.
Dr. Hwang emphasized the importance for all U.S. states and jurisdictions to participate in the registry so that national data could provide a better understanding of the causal pathways to SUID. Only with accurate and consistent data, can targeted interventions be developed to improve adherence to SUID-risk reducing infant care practices.
Overrepresentation of preterm infants and infants with recent illness in SUID cases
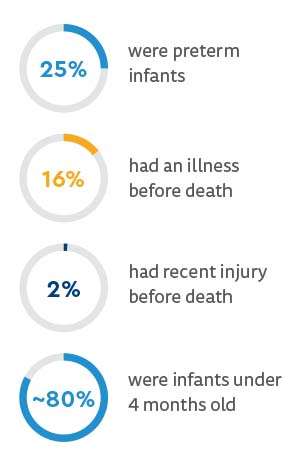
The study identified an overrepresentation of medically vulnerable infants in SUIDS cases, of whom likely had interactions with healthcare systems and clinical providers:
Dr. Hwang pointed out the significant opportunity for deeper engagement with caregivers to offer education and support focused on reducing SUID risks, including modeling safe sleep practices for infants who spend time in the neonatal intensive care unit or the general pediatrics wards, once they are medically stable.
Soft bedding linked to SUID from airway obstruction, underscores need for safe sleep environments
Study authors found that 72% of the 4,929 SUID cases reviewed occurred with infants in unsafe sleep circumstances.
A safe sleep environment was defined using two criteria:
- Infant was found supine on a firm sleep surface, including a crib or bassinet mattress, portable crib or pack-and-play; and
- Sleep surface was free of soft objects, loose bedding, bumper pads, or any objects that could increase the risk for suffocation.
The study grouped SUIDs into mutually exclusive categories: four categories for unexplained causes and one category for explained causes. The mechanisms for the explained or possible suffocation occurring in an unsafe sleep environment were specified in the registry as soft bedding, wedging/entrapment and overlay.
In SUID cases categorized as “explained” or “unexplained–possible suffocation,” 74% of airway obstructions were due to soft bedding. In her commentary, Dr. Hwang stated 1,145 infants may have survived their first year of life had soft bedding not been used during their sleep.
“This astonishing finding must propel healthcare providers, public health experts, policy makers and communities to work at individual, community, health systems and legislative levels to prevent these avoidable deaths”
- DR. HWANG
Dr. Hwang made three recommendations to improve safe sleep for infants:
- Consistent data collecting and reporting for all SUID cases
- Engaging families of preterm infants and infants with recent illness given their over-representation in SUID cases
- Advocating for the ban of infant products that are marketed for use during infant sleep but are unsafe
Research commentary conclusion: using data to identify risks and reduce SUID
Dr. Hwang closed her commentary with, “Only with robust, comprehensive and accurate data can we identify populations with greatest risk and understand causal mechanisms of suffocation to develop targeted interventions to finally move the needle on SUID rates that have seen no decline in over 20 years.”
Featured Researchers

Susan Hwang, MD, PhD, MPH/MSPH
Neonatologist
Neonatal Intensive Care Unit
Children's Hospital Colorado
Associate professor
Pediatrics-Neonatology
University of Colorado School of Medicine





 720-777-0123
720-777-0123










