The patient, a 17-year-old girl, lies anesthetized, very still. Her long hair drapes the lip of the operating table.
"Does anyone have a ponytail holder?" says Children's Hospital Colorado's Brent O'Neill, MD. Then Dr. O'Neill, a brain surgeon, combs the patient's hair.
The patient has suffered debilitating, near-constant seizures since she was 4 years old. Basically electrical storms in the brain, seizures originate from a central epicenter or lesion. Remove that lesion and the seizures stop.
Finding the storm
The tricky part is finding it. The storms spread at the speed of light, making their centers hard to target. By placing electrodes into the brain, doctors can record seizure activity over a week, locate the epicenter and take it out.
Those electrodes have to get there first. One placement method is to remove a section of the skull and place a grid of electrodes on the surface of the brain. This is less invasive and more precise than the craniotomy and grid is frame stereotaxy. That surgery involves essentially scaffolding a patient's head and mechanically calculating the exact location and angle to drill holes in the skull and then place electrodes one by one.
The problem is that each electrode can take a half hour or more to place, and over the course of placing 10 or 20, an operation can drag on for many anesthetized hours. It's hard on doctors and patients alike.
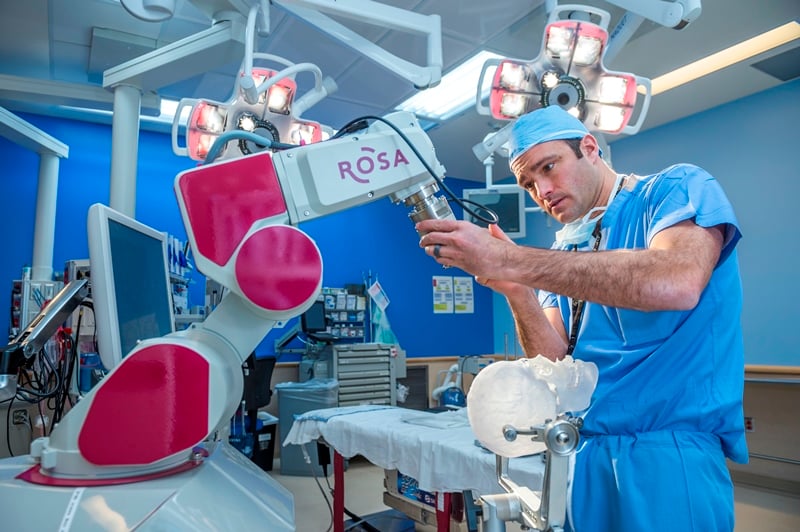
Dr. O'Neill's new surgical assistant, a robot called ROSA, cuts the placement time per electrode to five minutes. With the help of ROSA, one of only about 20 robots of its kind in North America, each step of the operation has been meticulously planned in advance.
ROSA's screen displays each site on images of the patient's skull, along with the evidence of a lobectomy she underwent at 10 years old: a ragged rectangle in the bone, held in place with titanium clips. It worked, but the seizures came back.
Increasing efficiency and minimizing risk
Now, Dr. O'Neill simply presses a foot pedal to align the robot with the next site. He can then drill the next tiny hole for introducing an electrode. By eliminating the need to constantly recalibrate, ROSA increases not only efficiency but also precision, minimizing risk.
Over the next week, epileptologists, along with a team of electrophysiologists and neuropsychiatrists, will isolate the epicenter and electrify electrodes of interest to prove the target area has no vital neurological function. Dr. O'Neill will remove the lesion. Once again, the patient will be seizure-free.
And they hardly even messed up her hair.
Learn more about the Neuroscience Institute at Children's Colorado.
Featured Researchers
Brent O'Neill, MD
Neurosurgeon
Children's Hospital Colorado





 720-777-0123
720-777-0123