What makes the Children's Hospital Colorado PICU so successful when it comes to saving even the most critical patients?
In late 2021, the Children’s Hospital Colorado pediatric intensive care unit (PICU) took on a case that wasn’t rare but was remarkable. The patient was a 15-year-old girl who sought care at Children’s Colorado for COVID-19. When she arrived, she had an oxygen saturation in the 70s, pneumonia, a pulmonary embolism and needed to be intubated. Her case was so severe, the team wasn’t sure she’d survive.
Starting on veno-venous extracorporeal membrane oxygenation (VV-ECMO)
At the beginning of the patient’s stay she was incredibly weak and could barely lift her pinky, says Aline Maddux, MD. Dr. Maddux was the primary PICU provider assigned to the patient, and it was her job to coordinate a multidisciplinary care team in seeking solutions to the complex case. To give the patient her best shot at survival, the team employed a support machine called veno-venous extracorporeal membrane oxygenation, or VV-ECMO, which takes blood from the body, oxygenates it, removes carbon dioxide and feeds the blood back into the venous system. Where most pediatric hospitals would require that the patient remain sedated with a breathing tube while on ECMO, the Children’s Colorado ECMO and PICU teams took a different approach. Fearing that a tracheostomy and a respirator would cause more damage to the patient’s sick lungs and prolong rehabilitation, the team made the bold decision to allow her to remain awake and active while on ECMO.
“She could eat, she could talk and she could participate more with rehab,” says Michele Loi, MD, who serves as the PICU’s Director of Quality Improvement. “Our PICU attendings spoke to several centers to gather information from adult colleagues on what they were doing and then ended up with this care plan that we carried out for several patients. This is very, very novel, especially on the pediatric side.”
According to Drs. Loi and Maddux, this approach was valuable not only in aiding physical recovery, but also in preserving the patient’s mental health. While her lungs were healing, the patient was able to see friends and family, visit other units to partake in therapy sessions (like baking brownies in the rehabilitation baking area), and share her ups and downs with providers. This focus on mental wellbeing isn’t always a standard of care in PICUs, often because patients are there for short stays or are unconscious for long periods of time. But Dr. Maddux says it made an incredible difference — enough to change her approach to future patients.
“When our patients are on such significant support as she was on, they’re usually not able to interact with us. And so, the only interaction we have is with their family and not directly with the individual because they can’t talk to us. But she could,” Dr. Maddux explains. “We understood what she was thinking, what she was feeling, what she was struggling with, and the obstacles and challenges that she was overcoming.”
To address these complex needs, Dr. Maddux held weekly meetings with over a dozen specialists from teams across the hospital, including occupational therapy, physical therapy, speech-language therapy, rehabilitation, pulmonology, child life, social work and the ECMO team. The meeting allowed each member of the patient’s care team to not only update others on their specific area of treatment, but also collaborate to address both physical and mental health needs and obstacles.
From utilizing an entire ECMO team (including cardiologists, cardiothoracic surgeons, interventionalists and ECMO specialists) who strategized constantly about her care and working with the early mobilization team to help keep her strong, to addressing the psychosocial well-being of both the patient and her family, the job of saving this patient truly took a village. And after several months in the PICU, she was well enough to return home just in time to attend her school’s prom.
An eye toward improvement
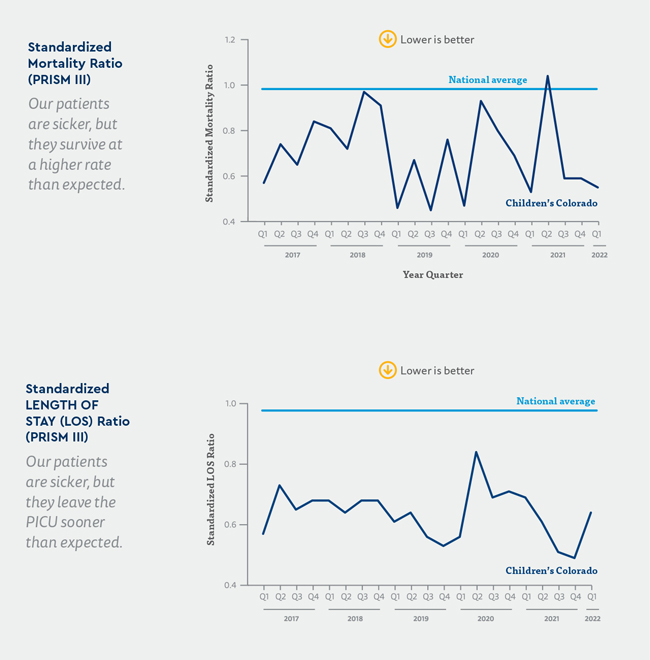
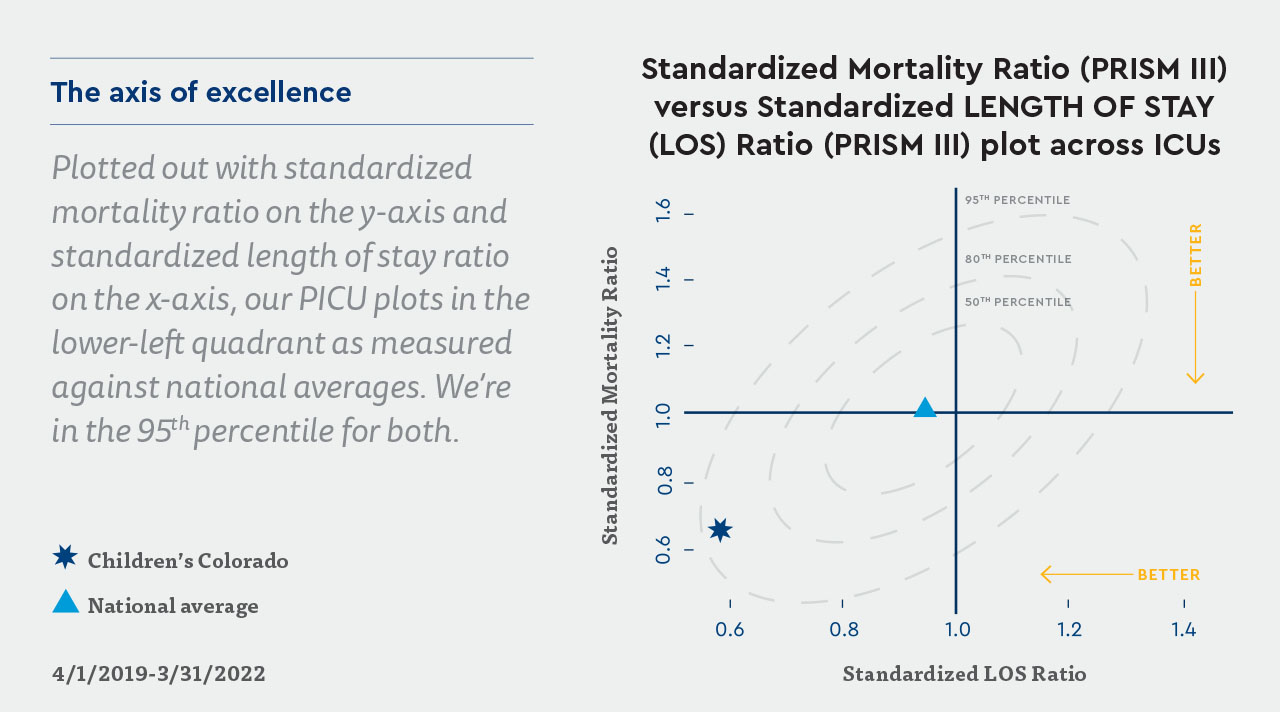
While this case is, in some ways, an outlier, it’s also a testament to the work the PICU has undertaken in recent years to focus on quality and process improvement. According to Dr. Loi and Cameron Gunville, DO, Medical Director of the PICU, these efforts contributed significantly to this patient’s positive outcome and have helped the Children’s Colorado PICU establish itself as a national leader in pediatric critical care. The team has found such success in focusing on constant improvement that it leads its peers in both standardized mortality ratio, which measures mortality against illness severity, and standardized length of stay ratio, which measures the length of stay against illness severity.
For this particular patient, numerous innovative approaches to care came together to build a successful outcome, starting with collaboration. According to Dr. Maddux, the sheer amount of time, energy and thought invested by so many different team members made all the difference in the 15-year-old’s recovery.
Dr. Gunville agrees: “It took huge coordination between the medical providers, nursing staff, the respiratory therapists, social workers, pharmacists, child life specialists and more. It takes so many people to collaborate and put all their effort into one person,” he says. “I think that’s why we’re as successful as we are. We have multiple teams that we work with and collaborate with in a multidisciplinary way. I think that’s hugely important.”
Beyond that indefatigable team effort, the patient also benefited from several nurse-led projects aimed at harm reduction and quality improvement. Led by Dr. Loi and nurses Sara Galt, RN, and Liz Diaz, RN, team members meet regularly to discuss potential concerns National average Children’s Colorado and strategize ways to address them. Recent projects have focused on reducing pressure injuries, bloodstream infections and UTIs caused by Foley catheters. Though avoidance is hard to measure, Dr. Maddux is confident that each moment of extra care resulting from such projects contributed to getting her patient home as quickly and safely as possible.
Additionally, the team made successful use of a new approach to care known as early mobilization. Early in her stay, when the patient was intubated and unconscious, providers used the PICU’s new set of guidelines to determine whether she would be a good candidate for early mobilization, which aims to manually keep a patient’s muscles moving, even while they are sedated or unconscious. Even that passive form of movement can lead to less muscle-tone loss and may ultimately facilitate a quicker recovery.
This case also inspired new areas for improvement, such as high-risk rounding. As part of this, the PICU built a team of providers and nurses committed to visiting patients with complicated cases to check in with bedside nurses, provide help where necessary and teach new skills on the fly.
“Hopefully because of this, we will prevent future hospital-acquired conditions,” Dr. Loi says. “We have data that shows that our rates of central line-associated bloodstream infections and pressure injuries [have decreased], specifically because of high-risk rounding.”
Leveraging PICU research
High-risk rounding is not the only change driven by this patient’s four-month stay in the PICU, according to Dr. Maddux, who also serves as the director of the PICU’s clinical and translational research program. The team participated in the national “Overcoming COVID-19” study, which tracks and characterizes complications resulting from COVID-19 in children.
And because of the difficulty the team members experienced measuring the recovery of this patient and others, they are seeking new solutions, including a device that evaluates recovery by measuring activity in kids as they get back to their everyday lives. The hope is to optimize the recovery period so patients can return to their previous activity level quickly, while also moving social and emotional recovery forward.
Cases like these, that involve intense collaboration among dozens of team members across a variety of disciplines, not only strengthen the case for teamwork, but also actively improve it. Dr. Maddux says that as a result of this patient’s stay, the PICU built strong bonds with the rehabilitation and pulmonology teams that have spawned new studies aimed at helping future kids.
“We’re launching a study that is going to look at pulmonary function recovery as well as physical recovery in children with bad lung disease who are in our PICU,” Dr. Maddux says. “This patient wasn’t a part of those studies, but as we were working with her, it brought up some of those questions and facilitated some of those collaborations.”
That constant drive to not only improve, but to back those improvements in process and treatments with data is something that sets the Children’s Colorado PICU apart, says Dr. Gunville.
“We have grant-funded basic and clinical science researchers, we have experts in quality improvement, experts in education. That’s a unique skill set to have at an academic center, and I think we all complement each other,” he says. “When you’re sending a kid to us, you’re sending a kid to a center of experts.”
Featured Researchers

Michele Loi, MD
Quality Director of the PICU
Children's Hospital Colorado
Assistant Professor
Pediatrics-Critical Care Medicine
University of Colorado School of Medicine

Aline Maddux, MD, MSCS
Director of PCCM Clinical and Translational Research
Pediatric Intensive Care Unit (PICU)
Children's Hospital Colorado
Assistant professor
Pediatrics-Critical Care Medicine
University of Colorado School of Medicine

Cameron Gunville, DO
Medical Director of PICU
Children's Hospital Colorado
Associate professor
Pediatrics-Critical Care Medicine
University of Colorado School of Medicine





 720-777-0123
720-777-0123