Key takeaways
-
Pediatric LDLT is not regularly performed in the U.S.
-
Pediatric LDLT is available at just a few centers across the nation.
-
This study compared pediatric waiting list and post-transplant outcomes by LDLT center volume.
-
High-volume centers were found to improve wait list survival; DDPLT and overall volume are linked with post-transplant survival.
Despite being the gold-standard treatment for children with end-stage liver disease, pediatric liver transplantation is complex and infrequently performed. In 2019, only 551 pediatric liver transplants were performed in the United States, while 8,345 adult liver transplants were performed.
Technical variance grafts, which allow a portion of an adult liver to be donated to a smaller pediatric recipient, is becoming increasingly important due to:
- Overall shortage in availability of deceased liver donors
- Continued decrease in pediatric deceased liver donors
- Need for size-matched grafts in this population
Technical variance grafts include:
- Reduced-size graft
- Split graft (one adult liver graft split into two grafts for use in one adult and one child)
- Low rates due to logistical issues, concerns about complications and higher failures
- Living donor liver graft
The option of living donor liver transplantation (LDLT) can increase the supply size-matched grafts for children and offers:
- Equal or better outcomes to deceased donor liver transplantation
- Low donor risk (small amount of liver needed for the pediatric recipient)
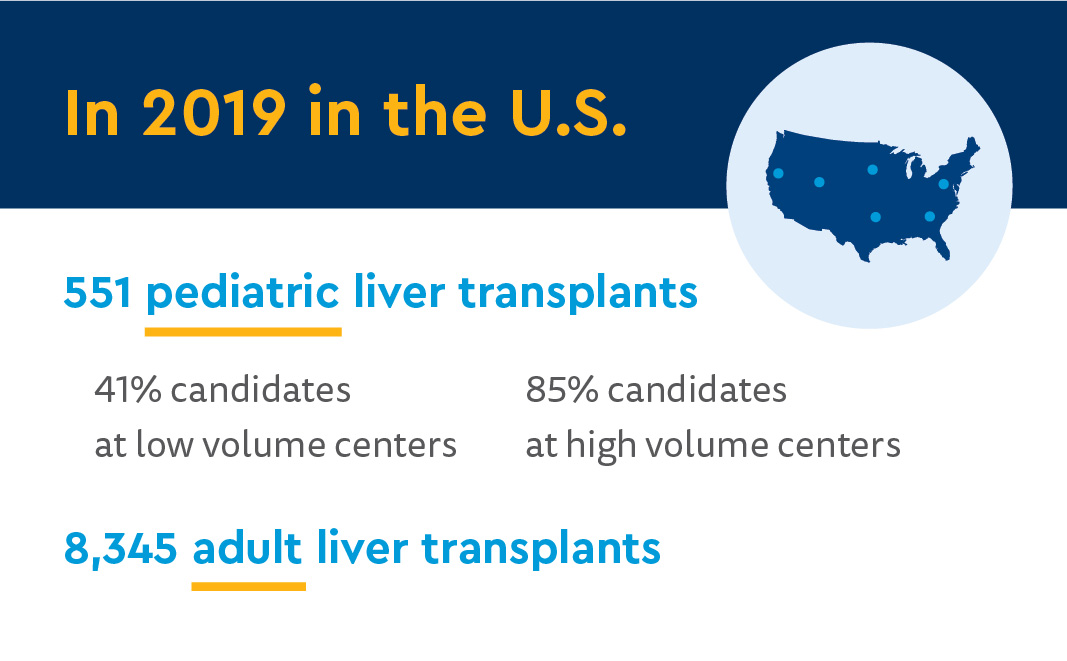
In adults, LDLT recipients in high-volume centers achieve superior outcomes, but the impact of LDLT center volume has not been studied in the pediatric population. This study compared pediatric waiting list and post-transplant outcomes by LDLT center volume.
Methods
Researchers from the Pediatric Transplant Program at Children’s Hospital Colorado conducted a retrospective review of the Scientific Registry of Transplant Recipients/Organ Procurement and Transplantation Network database.
Study population
- All pediatric liver transplant candidates <18 years old
- Listed Jan. 1, 2009 through Dec. 31, 2019
- Excluding:
- Re-transplantation or multiorgan transplantation
- Unknown listing center
- Excluding:
Researchers calculated:
- Annual number of LDLTs
- DDPLTs
- Overall liver transplants performed
- Waiting list dropout (death on list, de-listing due to condition)
- Association between center volumes and waiting list dropout, recipient death and graft loss
Results: associations with outcomes and survival
Transplant center volumes
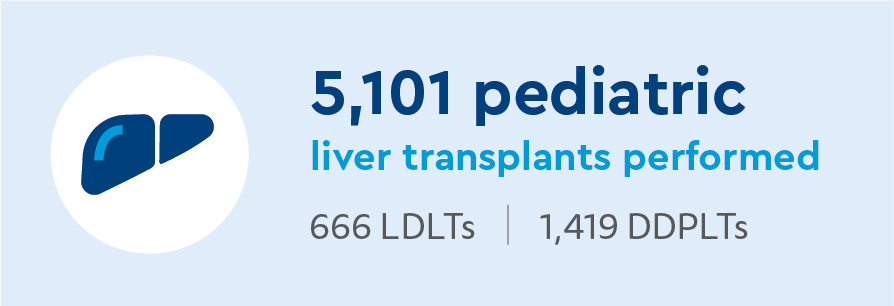
There were 88 transplant centers that listed at least one pediatric candidate during the study period. Of those:
- 5,201 pediatric liver transplants performed
- 666 LDLTs
- 1,419 DDPLTs
- Average annual LDLTs per center
- 0.69 ± 1.40
- 8.36 at center performing the most
- 1.47 ± 2.21 average DDPLTs per center per year
- 5.27 ± 6.90 average total pediatric liver transplants performed per year per center
- 34% of centers did not perform any DDPLTs
- LDLT center volume significantly correlated with DDPLT, total pediatric center volume
- DDPLT and overall center volumes strongly correlated
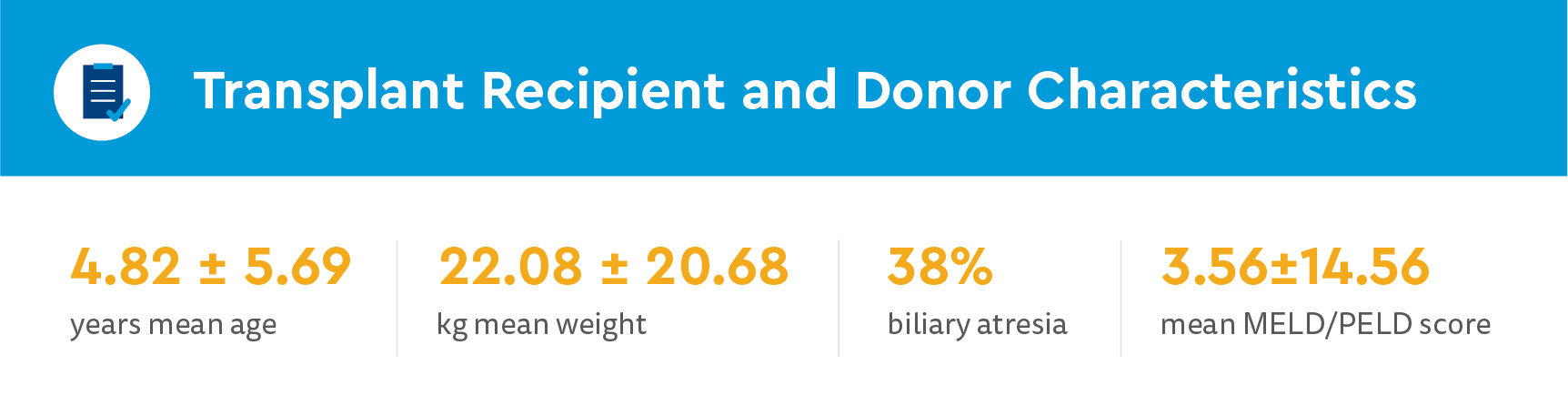
Transplant candidate characteristics
- 6,744 listed pediatric liver transplant candidates
- 4.81 ± 5.78 years mean age
- 22.20 ± 21.50kg mean weight
- Biliary atresia most common diagnosis at time of listing
- 6.24 ± 3.12-hour average cold ischemia
Waiting list outcomes
- 76% reached transplant
- 138.13 ± 247.06 average days on list
- 59 median days
- 18% removed (condition improvement, other reasons)
- 567.04 ± 728.14 average days on list
- 260 median days
- 7% waiting list dropout
- 124.75 ± 325.88 average days on list
- 27 median days
Associations between center volumes and waiting list dropout
LDLT center volume and private insurance were significantly protective against waitlist dropout. DDPLT and overall center volume were not protective.
Significant independent risk factors for waiting list dropout included other diagnoses, calculated and listing MELD/PELD score mechanical ventilation and dialysis.
Recipient survival
7% of recipients died a median 4.68 ± 3.29 years of follow-up.
Associations between center volumes and survival
DDPLT center volume was significantly and independently protective against death.
Hepatoblastoma, acute liver failure, "other” diagnosis, match MELD/PELD score and mechanical ventilation were significantly and independently associated with increased risk for recipient death.
Graft survival
14% of recipients experienced graft loss during a median 4.68 ± 3.29 years after transplant.
Associations between center volumes and graft survival
DDPLT center volume and overall volume were significantly protective against graft loss. LDLT volume was not protective for either.
Hepatoblastoma, acute liver failure, "other" diagnosis, mechanical ventilation and cold ischemia time were significantly and independently associated with increased risk for recipient death.
Discussion and conclusion: Expertise in all pediatric liver transplant options is important for best outcomes
Key study findings:
- Center volume of pediatric LDLTs significantly influenced waiting list outcomes
- Higher volumes protective against death on the waiting list or removal
- LDLT center volume not independently associated with post-transplant survival
- Overall and DDPLT center volumes protective against graft loss
- DDPLT center volume protective against death after pediatric liver transplantation
The study resulted in the new finding of a demonstrated pre-transplant waiting list survival benefit of LDLTs. This suggests availability of LDLT at a center may benefit all candidates listed at that center by decreasing the competition for size-matched deceased donor grafts.
Increasing access and listing, or multi-listing, at high-volume pediatric liver transplant centers with expertise in LDLTs and DDPLTs could optimize waiting lists and posttransplant outcomes. This could further grow the regionalization of specialized pediatric liver transplant care. As a prevalent and controversial issue –– possible lengthy distance of travel, concerns about access and socioeconomic disparities, etc. –– regionalization should be considered.
The researchers concluded that listing at a high-volume pediatric LDLT center can improve waiting list survival, while DDPLT volume and overall volume are associated with post-transplant survival. To optimize outcomes, having expertise in all options for pediatric liver transplants is important.





 720-777-0123
720-777-0123










