Key takeaways
-
Current standard surgical intervention for BA is Kasai hepatoportoenterostomy (HPE).
-
There is a debate around primary LT vs. HPE since LT is often ultimately necessary even after HPE relieves biliary obstruction.
-
Using a large, multi-institutional data set from the national Scientific Registry of Transplant Recipients (SRTR), researchers at Children’s Hospital Colorado compared primary and salvage LT outcomes for children with BA.
-
The study includes review of post-transplant and waiting list survival derived from post-MELD/PELD era.
-
HPE should remain standard of care as it may delay LT to after age 1 in a subset of patients and does not negatively impact later LT outcomes.
Stats
- 1 out of every 12,000 babies born in the U.S. has biliary atresia.
- Approximately 50% of these children require liver transplantation by age 2.
Research background: liver transplant outcomes for biliary atresia
Biliary atresia (BA) is the leading cause of end-stage liver disease (ESLD) leading to pediatric liver transplantation. Currently, the standard surgical intervention for BA is performing Kasai hepatoportoenterostomy (HPE) within three months of birth. In some cases, the surgery prevents or delays ESLD, but most of these children will experience progression of liver failure, eventually requiring salvage liver transplantation (LT).
Kasai HPE often makes a subsequent LT more difficult, and is associated with greater risks for bowel, biliary and infectious complications. There has been longstanding debate around primary liver transplant versus HPE, but most studies predate the Model for End-Stage Liver Disease (MELD)/Pediatric End-Stage Liver Disease (PELD) allocation system.
Researchers in Children’s Hospital Colorado’s multidisciplinary Pediatric Liver Center, collaborated to compare primary and salvage LT outcomes for children with BA since the implementation of MELD/PELD.
Research methods: review of primary and salvage liver transplant data in children with biliary atresia
For this retrospective cohort study, researchers reviewed the National Scientific Registry of Transplant Recipients (SRTR)/Organ Procurement and Transplantation (OPTN) database for all children with BA listed for transplant between March 1, 2002, and Feb. 28, 2021.
Exclusions
- Adults 18 years old or older
- Re-transplants
- Multi-organ transplant listings
- Listing age 5 years or older without documented previous abdominal surgery
Categorizations
Primary LT
- No previous abdominal surgery at time of listing
Salvage LT
- Previous abdominal surgery
- Considered early failure (EF) if 1 year old or younger at time of listing
- Considered late failure (LF) if older than 1 year at listing
Waiting list drop out
- Death on the waiting list
- Delisting due to becoming too sick to transplant
Post-transplant graft loss
- Death
- Re-transplantation
The threshold of statistical significance was a p-value of < 0.05.
Research results: improved survival in children who received Kasai procedure before liver transplant
Candidate characteristics
Of the 3,385 patients included in the study:
- 523 (15%) candidates had not undergone prior abdominal surgery and were listed for primary LT at an age younger than 5 years
- 2,862 (83%) of the candidates had undergone prior abdominal surgery (assumed to be a Kasai HPE for this analysis), and were listed for salvage LT
- 2,281 (67%) listed at 1 year of age or younger
- 581 (17%) listed at an older age
- Primary LT and salvage LT-EF candidates were much younger and smaller, had higher total bilirubin levels and MELD/PELD scores at listing compared to salvage LT-LF candidates
- Primary LT candidates more commonly female, less commonly white or privately insured
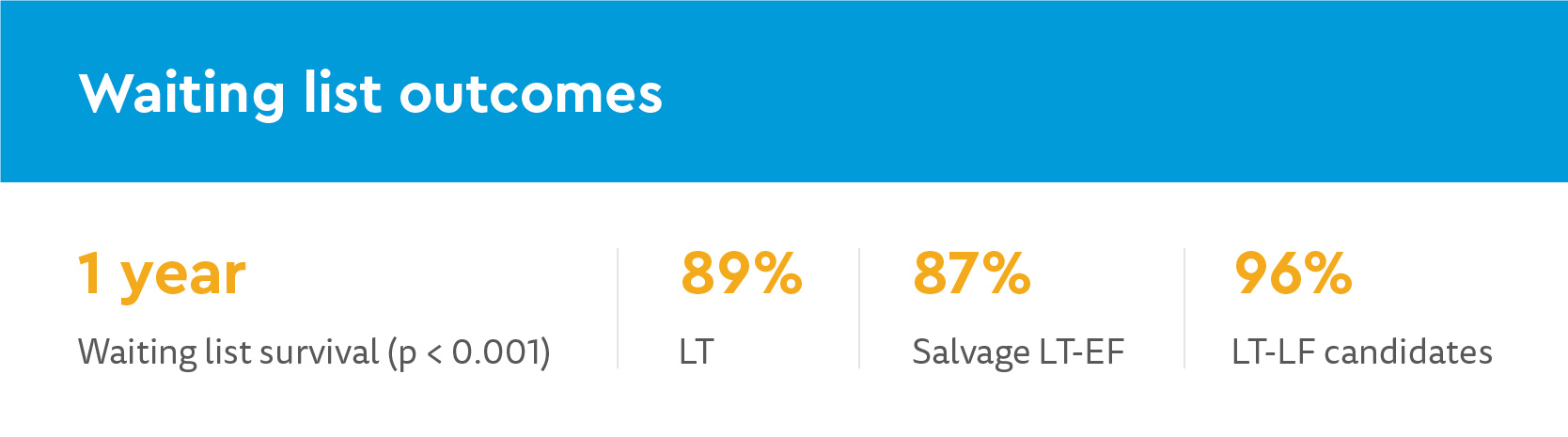
Waiting list outcomes
When waiting list drop-out was adjusted using multivariable Cox proportional-hazards model, there was no significant, independent difference in risk among primary and salvage EF or LF candidates.
LT recipient characteristics and post-transplant outcomes
Recipients of salvage LT-LF had lower bilirubin levels and were less critically ill, using MELD/PELD scores and hospitalization status. These recipients had higher waiting list and graft survival, but it was not statistically significant after adjusting using multivariable models.
There were no differences in waiting list, recipient or graft survival with primary vs. salvage LT after EF.
Research discussion: New data for pre- and post-transplant outcomes for children with biliary atresia
- Most children were listed for salvage transplant within the first year of life, after Kasai HPE with early liver failure
- After the first year, 15% listed for primary LT and 17% listed after Kasai HPE
- Primary and salvage LT-EF candidates and recipients had comparable outcomes
- LT-LF significantly improved waiting list and graft survival, but was not an independent predictor of survival after multivariable modeling
- Improved survival in salvage LF group could be due to:
- Lower bilirubin levels and MELD/PELD scores at listing
- Older age
- Greater weight
- Less frequent admission to ICU at time of transplant
This study supports literature describing no detrimental impact — and possible benefits — of HPE on pre- and post-transplant outcomes in this population. We make several critical contributions to the literature.
Due to the greater survival after Kasai HPE delayed transplant beyond first year of life, the study authors advocate for the current standard of HPE first followed by salvage LT if needed. This approach also:
- decreases competition for very small grafts from size-matched for infants
- could decrease waiting list times and mortality
- lowers healthcare costs compared to primary LT for BA
Authors note a concern in socioeconomic disparity, where more primary and salvage LT-EF candidates and recipients were of non-white race/ethnicity and had no private insurance.
Research conclusion: support for Kasai procedure for children with biliary atresia as standard of care
The study authors conclude Kasai HPE should remain the standard of care for children with BA. This procedure may delay the need for transplant beyond the first year of life or eliminate the need for LT in a small subset of recipients. Kasai also does not jeopardize later transplant outcomes, even in patients experiencing early failure.
Primary LT may be a reasonable option for the subset of children with BA destined for early failure, but validated tools to identify this subset of children are needed.
Featured Researchers

Megan Adams, MD
Pediatric Transplant Hepatology and Transplant Nephrology
Children’s Hospital Colorado
Associate Fellowship Director

Fritz Karrer, MD
Pediatric surgeon
Center for Children's Surgery
Children’s Hospital Colorado
Professor
Surgery-Peds Surgery
University of Colorado School of Medicine

Jonathan Roach, MD
Pediatric surgeon
Center for Children's Surgery
Children's Hospital Colorado
Associate professor
Surgery-Peds Surgery
University of Colorado School of Medicine

Shikha Sundaram, MD
Medical Director, Liver Program
Gastroenterology and Transplant Hepatology
Children's Hospital Colorado

Michael Wachs, MD
Chief of Abdominal Transplant Surgery
Pediatric Transplant Program
Children's Hospital Colorado
Professor
Surgery-Transplant
University of Colorado School of Medicine





 720-777-0123
720-777-0123










