Key takeaways
-
Our researchers studied intraoperative frozen section to determine if it was a reliable tool for diagnosing renal tumors in pediatric patients.
-
In the study, intraoperative specimen turnaround time for frozen section averaged 20 minutes.
-
Intraoperative frozen section was 89.4% accurate in the diagnosis of Wilms tumors.
Research background: Accuracy of frozen section pathology in pediatric renal tumor diagnosis
Renal tumors are the fourth most common tumors in children. While Wilms tumor is the most common, there are other tumors that can affect children and adolescents including renal cell carcinoma, clear cell sarcoma, mesoblastic nephroma and rhabdoid tumors of the kidney.
Treatment typically requires multi-modal therapy including surgery, radiation and/or chemotherapy. There are a variety of different treatment regimens, and selection of the modality depends on a combination of clinical data including:
- Patient age
- Tumor histology
- Tumor weight
- Disease stage
- Protocol guidelines
Although not always possible, it is ideal to consolidate all surgical care so that any needed invasive interventions occur under one anesthetic.
The use of intraoperative frozen section as a diagnostic tool has been studied extensively in adult literature, yet rarely in pediatric literature. Intraoperative frozen section could be used to guide the need for adjunctive surgical procedures and quickly provide information to a patient's family.
Researchers in the Department of Pediatric Urology at Children's Hospital Colorado studied the reliability of intraoperative frozen section for the diagnosis renal tumors in children and adolescents.
Research methods: Review of patient records spanned a decade
Researchers reviewed the electronic medical records of patients who underwent the following procedures between January 2005 and December 2015:
- Radical nephrectomy
- Partial nephrectomy
- Incisional biopsy for a suspicious renal tumor at the hospital’s tertiary referral center
Only intraoperative frozen section and final pathology were evaluated. Cohen’s kappa coefficient was used to assess the concordance rate between intraoperative frozen section and final pathology with regard to histologic subtypes, benign versus malignant pathology, and Wilms versus non-Wilms tumor classification.
Research results: Turnaround time was quick, with a good concordance rate between intraoperative frozen section and final pathology
Of these:
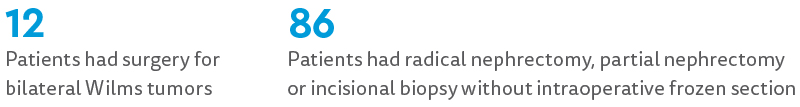
There were 32 patients who had intraoperative specimens submitted for intraoperative frozen section. Specimens submitted included:

Turnaround time was available for 29 patients. The median turnaround was 20 minutes, with 52% of intraoperative frozen section reports reported to the surgeon in less than 20 minutes.
Wilms tumor accounted for the majority of the cases (52%). The intraoperative frozen section correlated correctly in 82.1% of cases, incorrectly in 9.4% of cases, and was deferred to final pathology in 9.4% of cases.
Additionally:
- Overall histologic agreement between intraoperative frozen section and final pathology was determined to be good (kappa .071, 95% CI:0.52-0.899 P < 0.001).
- 94% of cases were correlated correctly when intraoperative frozen section was used to determine if a specimen was malignant or benign.
- Intraoperative frozen section correctly distinguished between Wilms and non-Wilms tumors 94% of the time.
- A total of 89.5% of Wilms tumors were correctly diagnosed with intraoperative frozen section.
Research discussion: Histologic diagnosis of renal tumors key to guiding need for adjuvant procedures at time of surgery
While intraoperative frozen section has been used for more than 100 years, with a diagnostic accuracy between 78 and 98% in pediatric solid tumors, it is used in less than 3% of pediatric renal tumor surgical specimens.
Clinical information including age, radiographic findings and intraoperative findings can aid in diagnosis, but often remains unclear until final pathology. This can result in patients undergoing unnecessary, incomplete or delayed procedures as part of their treatment.
It is important to establish a histologic diagnosis to guide the need for adjuvant procedures at the time of tumor resection. Intraoperative frozen section may rule out malignant tumor types that may require adjuvant chemotherapy. This can support decisions for or against vascular access placement during the same operative setting.
The study authors found the accuracy rates of intraoperative frozen section acceptable. With the quick turnaround time, the addition of intraoperative frozen section should have little negative effect to the ongoing procedure.
At Children's Colorado, close communication with the pathology team is stressed from the start of surgery, during its progress and if there are any pertinent intraoperative findings.
Research conclusion: Intraoperative frozen section a reliable diagnostic tool
Intraoperative frozen section appears to be a reliable and accurate tool for the following in children and adolescents with renal tumors:
- Establishing a histologic diagnosis
- Distinguishing between malignant and benign tumors
- Differentiating between Wilms and non-Wilms tumors
Communication between the surgeon and the pathologist is very important to ensure proper and efficient use of intraoperative frozen section. Study authors advocate for the use of intraoperative frozen section when obtaining a histologic diagnosis that will provide real-time guidance for medical decision-making and adjunctive surgical decisions.





 720-777-0123
720-777-0123











