Key takeaways
-
Researchers sought to learn more about the intestinal barrier of patients with inflammatory bowel diseases at the cellular level and how and if it is affected by the creatine transporter (CRT).
-
They studied the effect of knocking down and over-expressing CRT in intestinal epithelial cells (IECs) and mouse colonoids. They also measured levels of CRT expression in mucosal biopsies from patients with IBD.
-
They determined CRT is key to preserving the intestinal barrier and mucosal healing. Importantly, CRT expression is altered in colonic tissue of IBD patients. These findings could lead to important pathophysiological insights into IBD especially for ulcerative colitis (UC) and inactive Crohn’s disease (CD).
Research background: Determining if inflammatory bowel disease patients have altered creatine transporters
The chronic inflammatory disorder inflammatory bowel disease (IBD) can affect any part of the digestive system and is associated with a weakened intestinal barrier. Barrier integrity is mediated by tight junctions (TJ) between intestinal epithelial cells (IEC). Maintaining TJs is an energy consumptive process. During times of high energetic demand, the creatine-phosphocreatine cycle can support adenosine triphosphate (ATP) production. The cycle is dependent on intake of creatine by the creatine transporter (CRT). Previous research found creatine regulates energy distribution within cells and reduces the severity of colitis in mice.

Caroline Hall, MD, PhD, pediatric gastroenterologist in the Digestive Health Institute at Children’s Hospital Colorado and colleagues studied the effect of knocking down and over-expressing CRT in IECs, as well as evaluating the functionality of colonoids from CRT knockout mice. In order to investigate differences in barrier function, they explored differences in TJ activity and energy consumption. They also measured levels of CRT expression in mucosal biopsies from patients with IBD, a disease with notable barrier dysfunction. The study sought to determine if CRT plays an important role in preserving intestinal barrier and if CRT is altered in IBD patients.
Research methods: Analyzing the function of creatine transporters
Researchers analyzed intestinal biopsies from patients with IBD -- 30 with Crohn’s disease (CD) and 27 with ulcerative colitis (UC) -- and 30 patients without IBD (controls), an intestinal epithelial cell line and colon tissues from mice (with and without disruption of CRT), by immunofluorescence, immunoblots, and/or quantitative reverse-transcription PCR (qPCR). The patient samples came from the biobank repository at University of Colorado.
Research results: CRT regulates intracellular creatine, barrier formation and wound healing
In vitro results
- In T84 IECs with knocked down CRT (KD cells), there was an 80%reduction in CRT mRNA and a 50%reduction in protein. This resulted in a 50% decrease in intracellular creatine in KD cells, and supplemental extracellular creatine could not compensate for this difference.
- Staining for ZO-1, Claudin 1 and Claudin 2 in KD cells identified TJ protein localization within the cytoplasm rather than in the membrane at the TJs as in controls cells. Actin, which stabilizes TJ proteins, was mislocalized and showed less filament polymerization.
- Expression of TJ proteins was also affected as KD cells had a reduction of expression and protein concentration of Claudin 1 and an increase in expression of Claudin 2, a pore-forming claudin.
- Intestinal barrier integrity was leaky in the KD cells as indicated by lower TEER measures and increased FITC-dextran flux. These results were confirmed in CRT KO mouse colonoids.
- In a scratch test, KD cells healed the wound gap more slowly than control cells, identifying a wound healing defect.
- The KD cells failed to compensate with increased mitochondria respiration in response to metabolic stress. This suggests that KD cells are less resilient to stress.
- The over-expression of CRT in T84 cells (OE cells) produced a four-fold increase in CRT mRNA and a two-fold increase in protein. The increase in CRT resulted in a two-fold increase in intracellular creatine levels.
- In OE cells, Claudin 1 mRNA was not elevated, but Claudin 2 decreased nearly 50%. ZO-1 mRNA elevated two-fold. TEER and FITC-dextran studies identified stronger barrier function in OE cells.
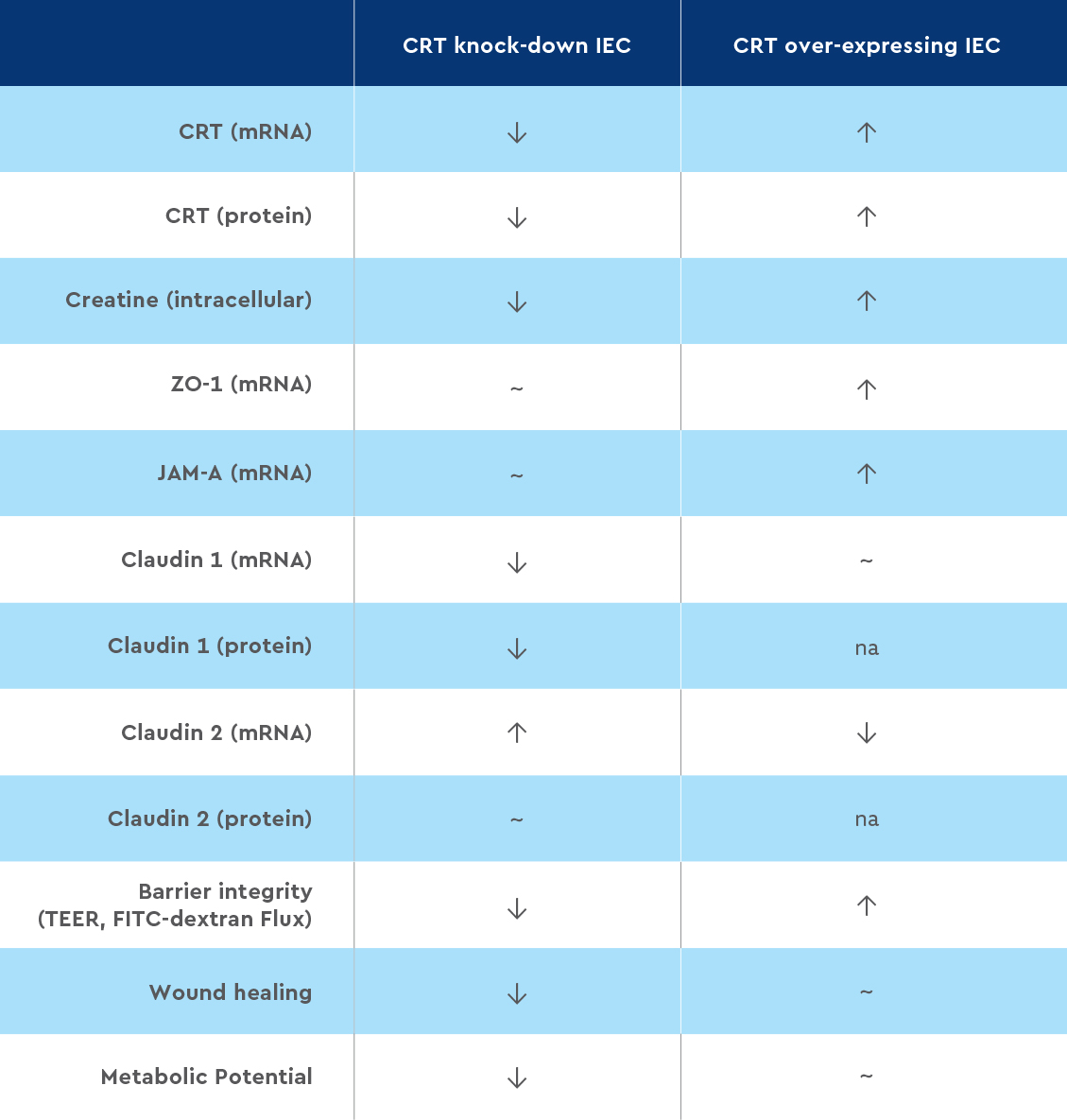
Table 1. Summary of in vitro results. Data is compared to control IEC cells. ↓ down regulated, ↑ up regulated, ~ similar expression as controls, na- not reported.
Biopsy results
- CRT was expressed in intestinal biopsies and was localized near TJs in IECs.
- Changes in CRT mRNA levels were a function of the type of IBD and disease activity. Tissue from active and inactive UC and inactive CD had lower CRT levels. CRT mRNA was similar in ileum and colon biopsies from CD patients.
- Increased CRT expression was related to increased Claudin 1 and decreased Claudin 2. There was no significant relationship between CRT and ZO-1.

Table 2. Summary of biopsy results. Data is compared to tissue from healthy controls. ↓ down regulated, ↑ up regulated, ~ similar expression as controls
Research discussion and conclusions: Reduced barrier function in IBD patients may be connected to lower CRT levels
Researchers found the down regulation of CRT in IEC produced a weakened epithelial barrier, likely due to changes in the TJ profile and localization. Knockdown IECs had low intracellular creatine. This suggests that extracellular creatine is the primary source intracellular creatine levels. If transport is impaired, the ability to respond to intestinal stressors is hindered and further weakens the intestinal barrier.
IBD patient biopsies supports that CRT may contribute to disease activity. CRT was decreased in UC and in inactive CD. Lower CRT expression was correlated with lower expression of Claudin 1, the “tight” TJ protein, and higher levels of Claudin 2, the “leaky” TJ protein.
These findings may provide important pathophysiological insights into IBD and in the differences between CD and UC.
Featured Researchers

Caroline Hall, MD, PhD
Pediatric gastroenterologist
Digestive Health Institute
Children’s Hospital Colorado
Assistant professor
Pediatrics-Gastroenterology, Hepatology and Nutrition
University of Colorado School of Medicine





 720-777-0123
720-777-0123