Key takeaways
-
Fecal incontinence and bowel disfunction are significant complications impacting many children with spina bifida or spinal cord injury.
-
This review resulted in the creation of new bowel management recommendations.
-
One recommendation is to use an abdominal radiograph as part of a bowel management strategy, which is not found in other current guidelines.
-
The review found the integration of the team into the clinic improved quality of life for these patients.
-
98% of patients with spinal cord injuries have at least one bowel related problem.
Background: bowel management needs in patients with spina bifida, spinal cord injury
Nerve impairment commonly causes bowel dysfunction in children with spina bifida (SB) or spinal cord injury (SCI). Managing bowel function is challenging and impacts the quality of life and well-being of these patients.
In addition to constipation and incontinence, secondary complications can include urinary conditions, shunt malfunction, skin breakdown, hemorrhoids and anal fissures, plus social and work problems. Patients with SB and SCI require a multidisciplinary, proactive and systematic approach to bowel management.
Current bowel management for constipation guidelines from the Spina Bifida Society call for education, dietary management and use of pharmacological agents. Recommendations not included in current guidelines:
- Abdominal X-rays to evaluate stool load
- Individualized enema plan before enema procedure (to keep children free from stool accidents)
- Antegrade continence enema procedure (ACE) combined with antegrade channel for Mitrofanoff procedure
The pediatric colorectal team in the International Center for Colorectal and Urogenital Care at Children’s Hospital Colorado has previous success with the above methods in patients with anorectal malformations and Hirschsprung disease, other conditions benefitting from bowel management interventions. They also saw success with SB patients who were referred to the team.
Given the need for a multidisciplinary, proactive and systematic approach to bowel management in patients with spina bifida and spinal cord injury, the colorectal team joined the multidisciplinary Spina Bifida and Spinal Cord Injuries Clinic at Children’s Colorado. In this paper, study authors shared key lessons learned from the integration of this specialized care team.
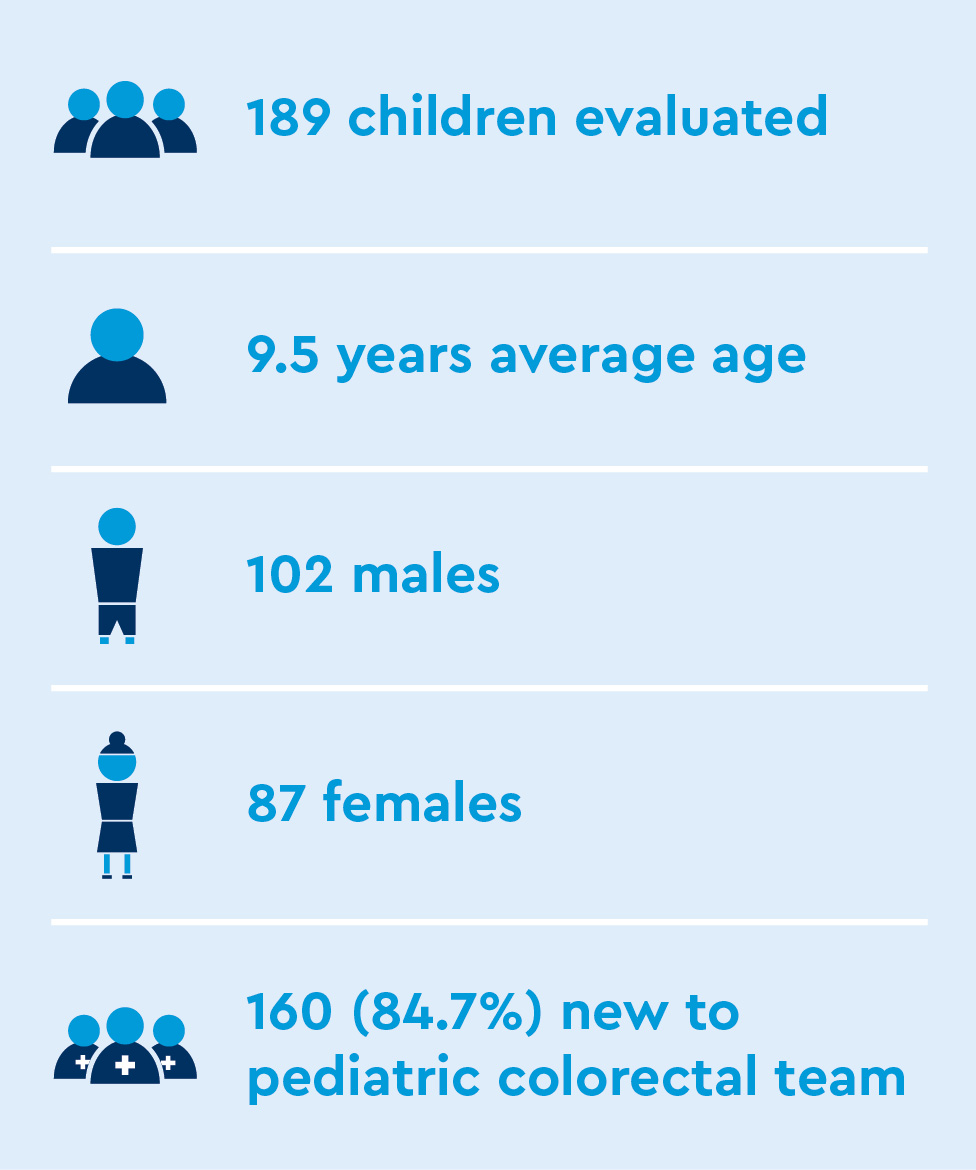
Methods: a retrospective review of medical records
The authors performed a retrospective review of electronic medical records of all patients seen at the clinic from September 6, 2020 to May 18, 2021.
They looked for specific outcomes including bowel and urinary continence, number of patients new to the team and characteristic findings on contrast enema.
Results: findings from retrospective review of spinal cord injury clinic patient
Diagnoses
- 153 SB
- 18 SCI
- 7 transverse myelitis
- 5 sacral agenesis
- 2 diastematomyelia
- 2 spinal stenosis
- 2 tethered cord with lipoma
Other clinical data
- 81 were wheelchair users
- 76.4% required regular enemas to be clean for stool (fecal incontinence)
- 68% required intermittent catheterization to be dry of urine
- 78.9% began bowel management at delayed age
- 54 patients had non-dilated, redundant colon in contrast enemas, distinct from other conditions
- 46 patients eventually received combined ACE/Mitrofanoff procedure to allow for antegrade catheterization of bowel and bladder
Discussion: colorectal team integration added specialized bowel management support
Many patients in this population were not being properly referred for bowel management. The integration of the colorectal team into the multidisciplinary clinic allowed for more streamlined care and better quality of life for patients.
The authors noted finding the right individualized enema pattern to keep patients clean from stool in their clothing can take time and dedication.
A contrast enema can help clinicians:
- Understand individual anatomy and characteristics of patient’s colon
- Estimate the enema volume required
- Find the right enema pattern and volume

Bowel management recommendations:
- Under age 3: MiraLAX® or Pedia-Lax® and larger enemas if not responding properly
- Age 3: formal bowel management with enemas
- Age 5 and beyond: combined ACE/Mitrofanoff procedure should be considered to allow for more independence
Conclusion: Specialized attention to bowel management is necessary for spinal cord injury and spina bifida patients
Study findings demonstrate the importance of specialized care for bowel management in pediatric patients with spinal cord injury or spina bifida. The incorporation of these experts into the multidisciplinary spina bifida and spinal cord injury clinic improved quality of life for these patients and their families.
Featured Researchers

Andrea Bischoff, MD
Pediatric surgeon
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Professor
Surgery-Peds Surgery
University of Colorado School of Medicine

Luis De La Torre-Mondragon, MD
Pediatric colorectal surgeon
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Associate professor
Surgery-Peds Surgery
University of Colorado School of Medicine

Hope Simmons, CPNP-AC
Certified pediatric nurse practitioner
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Instructor
Surgery-Peds Surgery
University of Colorado School of Medicine

Laura Judd-Glossy, PhD
Adolescent psychologist
Pediatric Mental Health Institute
Children's Hospital Colorado
Associate professor
Psychiatry-Child-CHC
University of Colorado School of Medicine
Alberto Peña, MD
Founding Director
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Professor emeritus
Surgery

Pam Wilson, MD
Pediatric rehabilitation specialist
The Orthopedics Institute
Children's Hospital Colorado
Associate professor
Physical Medicine and Rehabilitation
University of Colorado School of Medicine





 720-777-0123
720-777-0123