Condition and treatment background
Cloaca represents a range of defects, from benign with a good prognosis after a simple surgical repair to very complex cloaca malformations with many anatomic variations requiring different surgical maneuvers for successful reconstruction.
Until 2016, surgeons Andrea Bischoff, MD, and Alberto Pena, MD from the International Center for Colorectal and Urogenital Care at Children's Hospital Colorado, operated on the 570 pediatric patients for which this paper is based.
Benign patients require a meticulous and delicate repair, but will have bowel and urinary control, will become sexually active and can get pregnant and deliver via cesarean section. These patients represent more than 50% of all cloacas, and the surgical technique can be reproduced and taught to pediatric surgical trainees.
Conversely, complex patients with a common channel longer than 3 cm should have pediatric surgeons who are fully dedicated to repairing these malformations.
Newborn management
A cloaca diagnosis is made at birth by identifying a single perineal opening, usually found where the urethra would be. The genitalia of cloaca patients can range from almost normal looking for a less complex malformation to hypertrophic folds of skin, a flat bottom and an anal impression that is not well defined.
The first group tends to be the benign type with a channel less than 3 cm and good prognosis for future functions. The second group's presence of hypertrophic folds of skin often is misdiagnosed as intersex.
Within the first 24 hours of life and before surgery, important associated anomalies should be ruled out. The most important is the presence of a dilated vagina (hydrocolpos), which occurred in 38% of the newborns.
Despite sophisticated studies before the main repair, sometimes the entire anatomy can only be figured out during surgery, and that's when experience with the cloaca defect helps determine the appropriate surgical maneuvers.
After the colostomy has been opened and the hydrocolpos has been drained, the main repair should be done when the patient is stable, growing and developing normally.
Cloacas with a common channel
Shorter than 1 cm
These patients are treated very similar to those born with a recto-vestibular fistula and do not require total urogenital mobilization. There were 46 pediatric cases with a short common channel.
Length between 1 cm and 3 cm
Pediatric patients with a common channel shorter than 3 cm can be repaired through a posterior sagittal approach. There were 184 cases of this type.
Posterior cloacas
Posterior cloaca is a unique type of cloacal anomaly where the single opening is located at the normal location of the anus. Many pediatric patients have a normal anus, so surgical techniques should aim to keep the anus intact to preserve bowel function. There were 31 cases with posterior cloacas.
Length between 3 cm and 5 cm
The extent of the common wall between the urethra/bladder, vagina and rectum makes this type the most challenging group of anorectal malformations. In addition, the convergence of the three structures occurs in a difficult area. There are several maneuvers to gain extra length. In extreme cases, a vaginal switch or partial vaginal replacement may be necessary. There were 124 cases with cloaca that required vaginal replacement; and the segment chosen was rectum in 52, small bowel in 40 and colon in 32.
Length greater than 5 cm
Cloacas with a very long common channel have a shorter common wall between the vagina(s) and the urinary tract. Their repair can be challenging and a vaginal replacement is usually required. There were 119 cases in this category.
Re-operations
Patients with cloacas have one chance to receive the correct operation, and re-operation does not offer the same prognosis as the original repair. These are the most common types of re-operations needed in children with cloacas:
- Persistent urogenital sinus
- Acquired vaginal atresia or stricture
- Acquired urethral atresia or stricture
- Rectal prolapse
- Neo-vaginal prolapse
- Complex catastrophic complications (dehiscence, abscess and fistula)
There were 104 patients who underwent a re-operation.
Read the paper
Published in the April 2016 issue of Seminars in Pediatric Surgery.
Featured Researchers

Andrea Bischoff, MD
Pediatric surgeon
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Professor
Surgery-Peds Surgery
University of Colorado School of Medicine
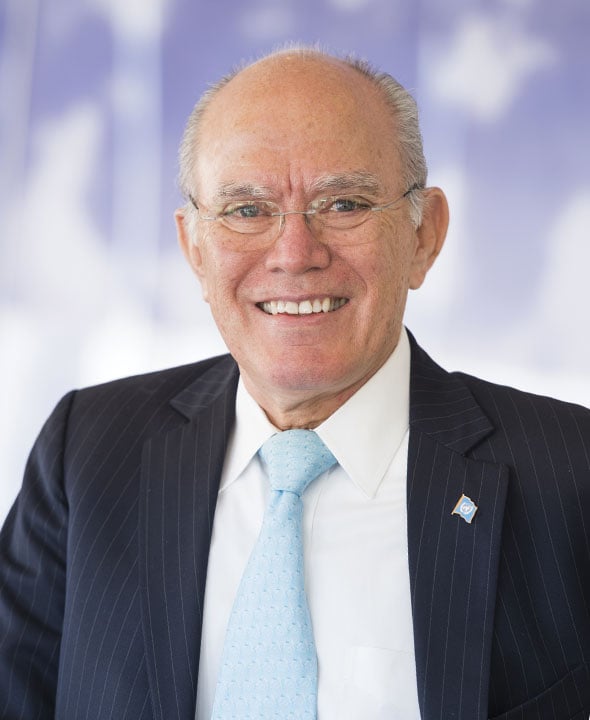
Alberto Peña, MD
Founding Director
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Professor emeritus
Surgery





 720-777-0123
720-777-0123










