Key takeaways
-
There is a lack of high-quality literature and there are no published guidelines for hemodynamic monitoring of critically ill children, except for the management of cases of shock.
-
An expert panel convened by ESPNIC created the first consensus-based recommendations for this population, excluding septic guidelines.
-
The recommendations should help guide clinical practice by showing which methods are more appropriate for follow-up of hemodynamic markers.
Stats:
- >50% of children with hemodynamic instability in intensive care units have multiple organ dysfunction
- No. 1 cause of hemodynamic instability is sepsis
- 94 recommendations written by expert panel
Research background: hemodynamic monitoring for detection and treatment of cardiovascular instability in critical care
Children in intensive care are commonly diagnosed with cardiovascular instability, which can include life-threatening conditions such as multiple organ failure and sepsis. It is well known that early detection and treatment of pediatric circulatory insufficiency or shock increases the chance of survival, but there is little data on how to best approach evaluation and monitoring of hemodynamic status in this population.
The best way to resuscitate children with circulatory failure is controversial because the methods are not backed by sufficient evidence. There is still debate about the best way to administer fluid or the type of vasoactive drug to use when a child enters this type of shock. If done correctly, hemodynamic monitoring should determine the severity of pediatric circulatory derangement and identify the root cause to inform the most appropriate treatment. It can provide useful information in the following scenarios of hemodynamic instability from:
- Major surgery
- Cardiac failure
- Trauma
- Sepsis
- Other causes of shock in children
Examining fluctuations in the instability and clinical goals are other aspects of treatment that are vital to ensuring successful treatment but have little evidence-based support. To address the wide gap in published literature, the Cardiovascular Dynamics Section of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC) created a working group to develop an expert consensus statement specifically for recommendations for pediatric hemodynamic monitoring.
Research methods: identifying pediatric hemodynamic monitoring experts and drafting recommendations
In addition to the three lead authors were nine members of the working group, all of whom have made significant contributions in pediatric hemodynamic monitoring. The requirements included previously published peer-reviewed research, working in a pediatric or neonatal intensive care unit, and experience with hemodynamic monitoring. Eduardo da Cruz, MD, the associate medical director of the Heart Institute and the head of Pediatric Cardiac Critical Care at Children’s Hospital Colorado, was one of the experts invited to participate in the working group.

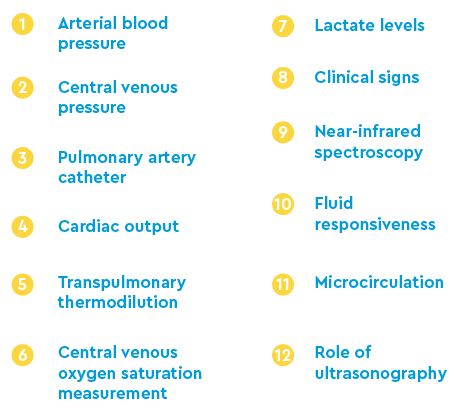
They were based on the reliability of methodologies, “normal” ranges and clinical usage of date for specific populations for 12 different subgroups (aspects) of hemodynamic monitoring.
Research results: finalizing recommendations for hemodynamic monitoring in chronically ill children

Research discussion: recommendations for pediatric hemodynamic monitoring organized by subgroup
The panel provided evidence-based support for all recommendations by subgroup.
Clinical signs
Being aware of the different signs in children that can help emergency responders and physicians identify that a child is in shock is extremely important, especially since many can go undetected.
Recommendation: Look at clinical, biochemical and monitoring signs that can signal pediatric hemodynamic instability.
Arterial blood pressure
Blood pressure is a common measure of hemodynamic instability, both high or low.
Recommendation: Use in conjunction with other easily observable clinical symptoms; evaluate on the basis of overall presentation and demographic factors like age, sex and body size.
Central venous pressure (CVP)
CVP can provide critical insight into pediatric hemodynamic instability, specifically when a child goes into shock post-treatment.
Recommendation: Look in the scope of the value and wave morphology when diagnosing, as well as its fluctuating response to any treatment given. Do not use CVP during the first phases of treatment; only in a shock refractory scenario.
Central venous oxygen saturation (ScvO2) measurement
ScvO2 measurement can be used when examining pediatric patients that may exhibit unstable symptomatology.
Recommendation: Watch closely as it can present as another condition and that may mask symptoms of hemodynamic instability. Use ScvO2 with other measures to help diagnose hemodynamic instability and guide treatment.
Volume resuscitation and fluid responsiveness
It is well known that administering too much fluid to a patient can cause significant harm.
Recommendation: Closely monitor perfusion indicators and clinical presentation before giving fluids. If central venous pressure begins to increase with no change in blood pressure or cardiac output, do not administer fluid therapy. Only use in situations where patients with an unstable presentation need early resuscitation.
Echocardiography/ultrasonography
Using less invasive methods to detect a patient’s hemodynamic condition is recommended, especially because it can provide a significant amount of information in a relatively quick amount of time.
Recommendation: Use cardiac ultrasound for a singular assessment rather than as a primary, regular measure in an intensive care unit. They can be used to detect and assess pulmonary hypertension, fluid responsiveness and understand other contributing pathologies.
Cardiac output (CO) monitoring and transpulmonary indicator dilution
For a stable patient, use ultrasound or a doppler-based process to measure CO. For an unstable patient, use only to initially investigate CO. The more unstable a patient is, the more invasive a procedure may be needed. In these cases, avoid more intricate or invasive forms of ultrasound due to feasibility.
Recommendation: Ultrasound methodologies are favored because they can be administered at a patient’s bedside and are noninvasive, which is helpful when working with children.
Pulmonary artery pressure (PAP)
A pulmonary artery catheter can provide useful information about a patient’s cardiac state.
Recommendation: Do not use this method on children due to the level of invasiveness it requires.
Lactate measurement
Using lactate measurements was highly recommended by the panel, especially in situations where a pediatric patient may be in shock.
Recommendation: Try to obtain a blood capillary sample from patients when the level is higher than 3.0 mmol/L. To make a diagnostic interpretation, use additional clinical observations, such as poor systemic perfusion and the monitoring of tissue perfusion parameters.
Near-infrared spectroscopy
While they recognized the practical use of near-infrared spectroscopy because of its noninvasive nature and ease to measure regional capillary-venous hemoglobin saturation, the panel did not recommend using this method in all children with hemodynamic instability.
Recommendation: Use only with pediatric patients who have recently undergone surgery for congenital heart defects.
Microcirculation
Not recommended; it is not feasible and comes at a much a higher cost than other methods to measure factors of hemodynamic instability.
Research conclusion: first hemodynamic monitoring recommendations of its kind
Besides septic shock guidelines, these are the first expert consensus recommendations created to guide clinicians.
Featured Researchers
Eduardo da Cruz, MD
Pediatric cardiologist
Children's Hospital Colorado





 720-777-0123
720-777-0123










