Key takeaways
-
There is a lack of evidence-based clinical guidelines to determine which infants with UPJO would benefit from pyeloplasty.
-
Lack of data leads to variance in criteria for surgery, rates of surgical intervention and care demographics among surgeons and centers.
-
Further studies should look at different ethnicities and a broader geographic range to help determine applicable criteria for treatments of infants with UPJO.
Stats:
- No. 1 cause of prenatally diagnosed severe hydronephrosis is UPJO
- <25% to ~60% range in surgical interventions at sites
- 1.2 months median age for initial urology clinic visit
Research background: identifying infants with UPJO and appropriate treatment
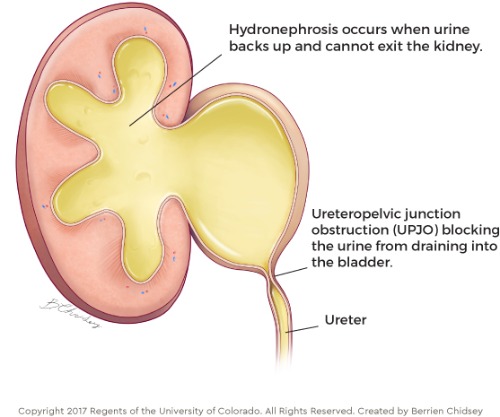
Ureteropelvic junction obstruction (UPJO) is a congenital condition that is often diagnosed before birth. It is a partial obstruction that occurs where the kidney and ureter meet, causing more urine to be produced than the ureter can drain. It is one of the leading causes of severe prenatal hydronephrosis, which is where urine builds up in the kidney leading to kidney dilation and possible kidney damage.
The severity of the disease and how it is treated varies from patient to patient. Although UPJO can be diagnosed prenatally via fetal ultrasound, it has been challenging for clinicians to distinguish between cases that will lead to kidney damage and those that will improve or resolve over time.
Additionally, there is a lack of guidance and criteria related to further assessments, treatment indications and surgical approaches, which could lead to demographic variations in care.
In this study, pediatric urology researchers from Children’s Hospital Colorado and two other children’s medical centers studied infants with UPJO to identify patient clinical and demographic factors associated with pyeloplasty.
Research methods: inclusion/exclusion criteria for infants with UPJO within the PURSUIT network
The hospitals are members of the PURSUIT (Pediatric Urologists Researching Surgical Outcomes Using Health Information Technology) network, which includes multiple academic pediatric urology practices. The network aims to facilitate collaborative data collection and analysis to establish best practices for congenital anomalies of the kidney and urinary tract.
Data collection

Inclusion criteria
- Patient of PURSUIT network pediatric urologist between 2018-2019
- Less than 6 months old at the initial visit
- Isolated unilateral SGU grade 3-4 hydronephrosis without ureteral dilation on initial postnatal ultrasound
Exclusion criteria
- Extraneous medical conditions that could interfere with the interpretation of clinical procedures for UPJO
- Prior kidney surgery
Imaging
Main urologic imaging technologies:
- Ultrasound at initial pediatric urology visit
- MAG-3 (administered via IV and urethral catheter with and without anesthesia)
Statistical analysis
Primary outcome measures were pyeloplasty within one year of the initial visit and SFU grade of hydronephrosis on the most recent ultrasound within the first year. Other covariates assessed were:
- Age at initial visit
- Race/ethnicity
- Treating site
- Insurance type
- History of febrile urinary tract infection (UTI)
- Initial ultrasound findings
- MAG-3 findings, if performed
Research results: patient demographics and characteristics associated with pyeloplasty

Patient characteristics
- Racial and ethnic distribution:
- 39.6% Hispanic
- 38.1% white, non-Hispanic
- 8.8% Black
- 5.4% Asian
- 12.9% other
- Insurance status: 58.3% private insurance
Initial presentation
- All initially diagnosed prenatally
- 5% had a febrile UTI before the first assessment
- 59.4% had an ultrasound at follow-up
- 56.9% had a MAG-3 study; 34.6% had a follow up MAG-3
Demographic and clinical factors associated with infant pyeloplasty
- 19.3% underwent pyeloplasty.
- The median time to pyeloplasty from the initial visit was 2.6 months.
- Infants at site C had the most pyeloplasty procedures at 28.8%.
- Of infants who underwent pyeloplasty, 78.9% had at least two visits and 58.8% had two ultrasounds before surgery.
- Of infants who had at least two ultrasounds before surgery, only 40% had worsening hydronephrosis per physician report; the remainder had stable ultrasound findings.
- 29.9% of infants had a Society for Fetal Urology (SFU) classification score of 4 on initial ultrasound.
- Infants evaluated with MAG-3 (29%), especially those with a T1/2 that was greater than 20 minutes, were more likely to have surgery.
Research discussion: clinical relevance of demographic characteristics for UPJO cases that need treatment
To date, the study is the largest to investigate clinical and demographic factors associated with infant pyeloplasty at a multicenter level.
Key findings
- Infant pyeloplasty varies greatly by practice, indicating uncertainty about what could be considered “ideal” criteria for surgery.
- A physician’s personal and clinical experience may play a significant role in whether a patient receives surgery as treatment.
- Procedures like MAG-3 may help to establish baseline functioning and determine patients who may benefit from surgery
- Although differential renal function is a measure of kidney damage, T1/2, an indicator of kidney drainage, was more highly associated with surgery in this study.
- Hispanic children were more likely to receive surgical treatment.
Significant study limitations
- Representation of other ethnic backgrounds
- Lack of a language difference analysis
Research conclusions: implementing systems to identify infants with UPJO for treatment
Despite the study’s limitations, several factors were identified as potential indicators for surgery as a treatment for infants with UPJO, such as prolonged T1/2. Both surgery and observation had similar rates of improved hydronephrosis.
However, there is still a significant gap in the clinical knowledge necessary to establish the effect of surgery on renal function and an ongoing need to standardize how these patients are evaluated, two essential steps in the development of evidence-based guidelines for surgery.
Future studies should look at a broader range of ethnic and racial backgrounds to better understand possible demographic differences in care and should establish a standardized process to track initial, short-term and long-term kidney function to define the association between surgical treatment and renal outcomes.
Featured Researchers

Vijaya Vemulakonda, MD
Pediatric urologist
Department of Pediatric Urology
Children's Hospital Colorado
Professor
Surgery-Urology
University of Colorado School of Medicine

Allison Kempe, MD, MPH
Director, ACCORDS, Anschutz Medical Campus
Ergen Family Endowed Chair in Pediatric Outcomes Research
Children’s Hospital Colorado
Professor of Pediatrics, Division of General Academic Pediatrics
University of Colorado School of Medicine





 720-777-0123
720-777-0123










