How has the field of vascular anomalies evolved to take on the most mysterious conditions?
For generations, pediatricians have relied on a “wait and see” approach when faced with the presence of a vascular anomaly, a functionally impactful birthmark or growth made up of vessels that develop incorrectly. Historically thought of as innocuous blemishes of little concern that fade as a child grows, many lesions can significantly impact a child’s quality of life. Vascular malformations and tumors — made up of abnormal capillaries, veins, arteries and lymphatic vessels — can be invasive, disfiguring and sometimes life-threatening. These vascular anomalies have long puzzled medical professionals, and the patients have lacked any sense of a medical home, creating a fragmented approach to care. Over the past decade, Children’s Hospital Colorado has transformed the treatment of vascular anomalies through a multidisciplinary approach that standardizes care and advances our knowledge of these complex vascular conditions. This effort is spearheaded by experts, including Taizo Nakano, MD, medical director of the Vascular Anomalies Center at Children’s Colorado.
A paradigm shift
Many vascular anomalies are considered medical mysteries that don’t fit neatly into any specific medical category. Patients and families find themselves shuffled between subspecialties and between diagnoses. The field historically lacked clear terminology and standards of practice, resulting in excessive or inappropriate therapies, pushing doctors and researchers to shift their thinking regarding these conditions. Children’s Colorado has collaborated with national and international colleagues to create a new practice from scratch — from developing a new classification system to developing consensus guidelines and establishing the academic infrastructure for clinical trials.
This new multidisciplinary approach to treating vascular anomalies was spearheaded by the collaborative leadership of Annie Kulungowski, MD, of pediatric surgery, Aparna Annam, DO, of the Department of Pediatric Interventional Radiology and Imaging, and Taizo Nakano, MD, of the Center for Cancer and Blood Disorders.
“The goal was to create a multidisciplinary medical home for patients with vascular anomalies, bringing experts together from various fields into the same room to expedite more accurate diagnoses and personalized treatment plans,” Dr. Nakano says.
Multidisciplinary model and the role of interventional radiology
The Vascular Anomalies Center has collaborated with most subspecialties available at Children’s Colorado to create a comprehensive medical home for patients with vascular anomalies. The core team includes pediatric surgery (general, plastic and ENT), interventional radiology, dermatology, hematology/ oncology, physical therapy and genetics. Depending on the location of the lesion, providers in additional subspecialties volunteer time to collaborate, including orthopedics, cardiology, GI, neurology and neurosurgery.
Therapeutically, the role of surgery has decreased over time due in part to the rise of interventional radiology, which often allows for more focal, minimally invasive treatment.
“Interventional radiology is now an essential part of the multidisciplinary team, and efforts are made to increase recognition and support for this field within the institution,” Dr. Nakano says. “The recent addition of two new state-of-the-art interventional radiology suites and the recruitment of new faculty have helped interventional radiology keep up with the demands of this growing field.”
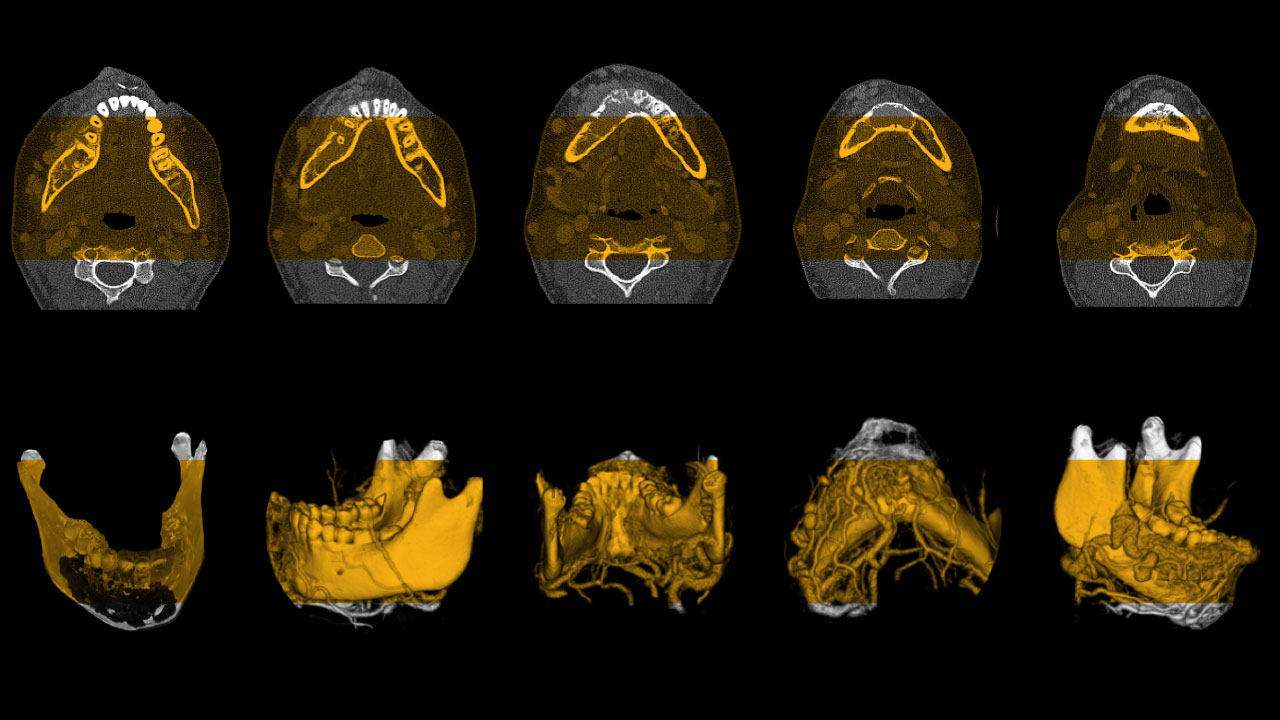
This multidisciplinary approach also led to the development of a disease classification system that goes beyond the physical exam, incorporating clinical, radiographic, pathologic and genetic features to define any given vascular anomaly. This system allows for a more accurate diagnosis and targeted, personalized treatment options, ultimately improving outcomes for patients with vascular anomalies.
“We can now describe anomalies by more than just physical appearance. We include radiographic and histologic features and sequence to identify the genetic drivers of these progressive, dynamic anomalies,” Dr. Nakano says. “As a team, we each contribute our skillset to add layers and depth to the diagnosis, which results in expedited and accurate diagnoses and opens the door to more targeted therapy options.”
Although the field of vascular anomalies is rapidly evolving, many conditions have still not yet been thoroughly studied, leaving gaps in knowledge that must be addressed.
International collaboration
In collaboration with the Hendren Project, an online global community of pediatric surgeons and urologists, Drs. Nakano and Kulungowski host a “Multidisciplinary Approaches to Vascular Anomalies” webinar series. They originally developed the series to facilitate international discussions regarding the evaluation and management of vascular anomalies, stressing the importance of a multidisciplinary approach. Additionally, they have collaborated with industry to develop an educational curriculum, allowing them to share patient stories and highlight the shift from clinical, radiographic and pathologic thinking to a more genetic-based approach.
In recent years, the field has caught pharmaceutical companies’ attention, leading to advancements in the field’s first interventional trials to develop targeted pharmacotherapy treatment options. One such example is the FDA approval of alpelisib, a drug initially developed for breast cancer that can treat a large cohort of vascular anomalies known as PIK3CA-related overgrowth spectrum, providing hope for patients and families affected by these conditions.
The role of lymphatics
The lymphatic system is an extensive and intricate network of vessels that drains the fluid from soft tissues, circulates through lymph nodes and returns to the heart. It plays a vital role in transporting proteins from the gut and is closely intertwined with the body’s blood vessels. Despite its importance, no single medical subspecialty has traditionally taken ownership of lymphatics, leading to a gap in understanding and treating lymphatic-related diseases. However, work on vascular anomalies is now shedding light on this essential and complex system, leading to breakthroughs in the understanding and treatment of various vascular disorders related to the lymphatic system.
A notable example of Dr. Nakano’s collaborative efforts in the lymphatic space is the treatment of children with Noonan syndrome, a developmental condition with over-active germline genetic defects in the RAS/ MAPK pathway that affects the entire body. In addition to cardiac and developmental disorders, patients with Noonan syndrome often suffer from lymphatic anomalies in and around their lungs that risk a catastrophic lymphatic leak. Katie Chatfield, MD, a cardiologist and geneticist at Children’s Colorado, worked with the vascular anomalies team to explore the possibility of repurposing known inhibitors of this over-active pathway to treat life-threatening presentations.
The treatment involved a medication called trametinib, obtained through compassionate-use access, which required approval from the drug company, the FDA, Children’s Colorado and the patients’ guardians. To date, the treatment has proved successful, helping patients with their lymphatic issues and improving their overall health — including growth, cardiac function and appetite.
The team’s approach to treating Noonan syndrome is moving beyond single-patient trials and towards expanded national collaborations with other subspecialties and institutions. This work has the potential to transform the understanding and treatment of various disorders related to the lymphatic system, opening up new avenues for research and therapy.
“While the ethics and logistics of treating young children and infants with targeted inhibitors are complex, the possibility of significantly improving the development of a child with Noonan syndrome and limiting life-threatening complications is an exciting prospect,” Dr. Nakano says. “This is what makes academics fun. This is what keeps it interesting.”
Improving vascular anomalies care
The Vascular Anomalies Center has grown considerably in the past decade. Its support staff, including advanced practice providers, nurses and a clinic coordinator, help care for vascular anomalies throughout the greater Rocky Mountain region. With the expanded use of telehealth and taking advantage of the large multidisciplinary clinic space at Children’s Colorado, more patients can be seen, and demand continues to grow. Dr. Nakano and his colleagues’ work has profoundly impacted patient care and how other medical fields may approach similar conditions.
“We have not only given a home to those diagnosed with vascular anomalies but also provided more satisfying explanations and treatment plans for those with previously unexplained conditions,” Dr. Nakano says. “As the field continues to grow and evolve, I hope that more effective treatments and a greater understanding of these rare conditions will become available, improving the lives of countless patients and families.”
Featured Researchers

Taizo Nakano, MD
Medical Director
Vascular Anomalies Center
Children's Hospital Colorado





 720-777-0123
720-777-0123