Key takeaways
-
Data collected from patients who received EXCOR from 2018 to 2020 were compared to patients who received EXCOR from 2007 to 2014.
-
Multiple, significant improvements in morbidity and mortality were found when comparing results from the historical cohort.
-
The findings may be the result of changes in patient care practices over time and collaborative learning.

In this study:
- 86% success rate in post surveillance study (PSS) group
- 44% reduction in stroke in post-surveillance study (PSS) group
Research background: Berlin Heart EXCOR for end-stage pediatric heart failure
The Berlin Heart EXCOR Pediatric (EXCOR) ventricular assist device (VAD) is the most used VAD for pediatric patients with end-stage heart failure. It was introduced in North America more than two decades ago, and until recently, there have not been significant changes in the management of these patients. The fundamental shift in approach to anticoagulation strategies coincided with a surveillance period required by the Food and Drug Administration (FDA) for its post-market approval (PMA) of the EXCOR in 2017.
This surveillance study re-analyzes the effectiveness of EXCOR. It also provides a comparison to the historical patient characteristics and outcomes of previous studies.
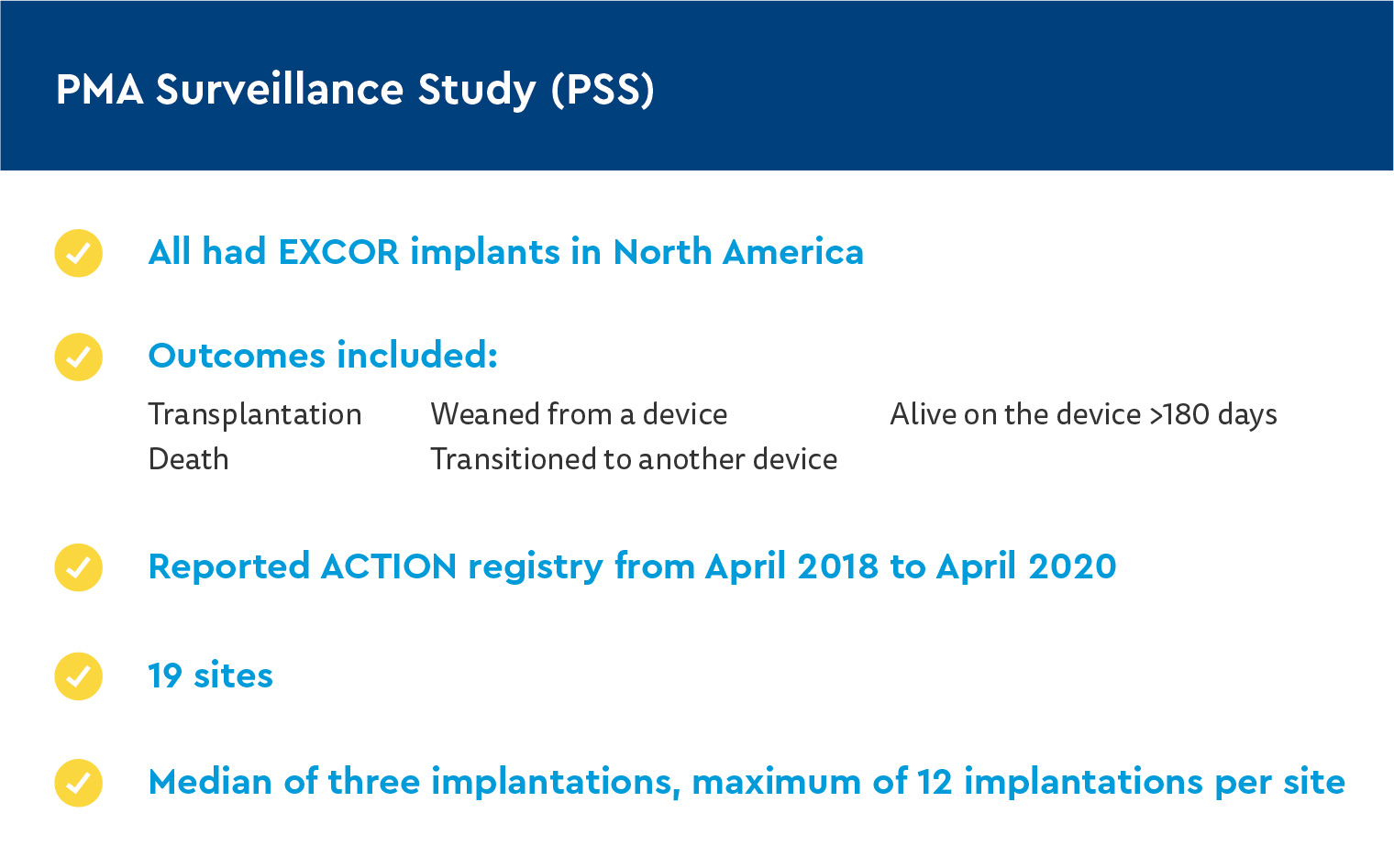
The international Advanced Cardiac Therapies Improving Outcomes Network (ACTION), which aims to improve outcomes on mechanical support in pediatric and congenital patients, conducted the PMA surveillance study (PSS). The PSS report summarizes the outcomes of patients supported with EXCOR from the ACTION registry. It also compared previous reports on a historical cohort of EXCOR patients.
Research methods: ACTION network Berlin Heart EXCOR comparative study groups
The Heart Institute at Children’s Hospital Colorado, which includes the Ventricular Assist Device Program, is one of 40 centers participating in ACTION. The ACTION registry collects and contributes data including mortality rates and neurologic dysfunction. Nineteen centers, including Children’s Colorado, had patients with EXCOR who met the criteria to supply data to the ACTION registry and PMA surveillance group.
Patient groups
PMA Surveillance Study (PSS)
The Berlin Heart Study (BHS)
- Data from this group used as a comparison
- Cohort included three sources
- Data from 320 patients who received EXCOR implant between 2007 and 2014
Definitions
- Primary outcomes determined 180 days after implantation
- Success defined as transplantation, weaned off the device for recovery, or alive on device therapy
- Adverse events only counted if patients supported with EXCOR
Statistical methods
- Categorical data presented as frequencies and percentages
- Continuous data presented as median and interquartile range (IQR)
- Fisher’s exact test and non-parametric Kruskal-Wallis test used to analyze categorical and continuous data
Research results: Berlin Heart EXCOR outcomes for PSS and BHS groups
PSS group
There were 72 total patients, representing 6,702 days of EXCOR support.
Demographics can be found in Table 1.
| Table 1 Baseline Characteristics of the PSS Group in Comparison With Those of BHS Group | |||
| Variable | BHS group, n=320 | PSS group, n=72 | p-value |
| Age, months, median (IQR) | 20.5 (6.9-77.5) | 9.0 (3.2-35.7) | 0.002a |
| Weight, kg, median (IQR) | 10.7 (6.9-18.4) | 8.0 (4.9-13.5) | 0.001a |
| BSA, m2, median (IQR) | 0.50 (0.36-0.78) | 0.40 (0.28-0.58) | 0.001a |
| Male, n (%) | 162 (50.6) | 32 (44.4) | 0.364 |
| Device type, n (%) | <0.001a | ||
| LVAD | 175 (54.7) | 37 (51.4) | |
| SVAD | 26 (8.1) | 18 (25.0) | |
| BiVAD | 119 (37.2) | 17 (23.6) | |
| Previous ECMO | 123 (38.4) | 17 (23.6) | 0.020a |
| CHD | 91 (28.4) | 33 (45.8) | 0.005a |
| INTERMACS profile, n (%) | 0.002a | ||
| 1 | 154 (48.1) | 20 (27.8) | |
| 2 | 152 (47.5) | 40 (55.5) | |
| 3 | 11 (3.4) | 9 (12.5) | |
| Abbreviations: BHS, Berlin Health Study; BiVAD, biventricular assist device; BSA, body surface area; CHD, congenital heart disease; ECMO, extracorporeal membrane oxygenation; INTERMACS, Interagency Registry for Mechanically Assisted Circulatory Support; IQR, interquartile range; LVAD, left ventricular assist device; PSS, post-market approval surveillance study; SVAD, systemic ventricular assist device. ap-values that are significant (<0.05). |
|||
- Of the 46% of patients with congenital heart disease (CHD):
- 54% had single ventricular physiology
- 79% had previous cardiac surgery
- 28% were INTERMACS Profile 1
- 30% were on ECMO at time of implantation
- 21 patients had previous device support before or after using EXCOR support
- All patients received anticoagulation management at the initial phase of post-implant care, majority treated with Bivalirudin (92%)
Outcomes were as follows:

- Of those:
- 3% recovered
- 17% alive on the device > 180 days of implantation
- 11% transitioned to different device
- 12.5% of patients died on the device
- Of the patients who survived:
- 16.7% experienced neurologic dysfunction (including stroke, extra-axial hemorrhage, transient ischemic attack and hypoxic-ischemic encephalopathy)
- 13% experienced major bleeding events and infection
- 27 pump exchanges took place with 17 patients, with the first replacement taking place at an average of 23 days after EXCOR implantation
Comparisons with Berlin Heart study (BHS) group
When compared to BHS group, the PSS group were younger, smaller, required to be supported longer and more likely to have CHD.
In addition:
- 92% had Bivalirudin as primary anticoagulation therapy
- Less likely to have bi-VAD and INTERMACS Profile 1 at implantation
- Success rate was 86% vs. 76%
- Fewer patients experienced a neurologic event:
- 44% reduction in stroke (5.3% vs 15.9%)
- Major bleeding (9.7% vs 38.8%)
- Major infection (18.1% vs. 35.3%)
- 44% reduction in frequency of pump exchange
- All other adverse events reduced
Research discussion and conclusion: Berlin Heart EXCOR outcomes have improved
As VAD therapy has evolved and more devices become available to treat heart conditions, so have the ways practitioners can use it to help save patients’ lives.
Key Findings
- Despite the difference in demographics of the PSS group, specifically, the higher-risk characteristics, both survival rates and incidence of AEs were improved.
- Results indicate an evolution in the experience of the pediatric VAD community, including earlier implant strategies and avoiding the need for right heart support or other complications associated with critical cardiogenic shock.
- EXCOR is a good option for pediatric patients with borderline BSA for durable continuous-flow VADs.
- CHD was more prevalent in the PSS group, indicating although it is still a risk factor for mortality after VHD implantation, it may not be as significant as it was once thought to be.
- There was a significant improvement in rates of early neurologic dysfunction, including stroke – reflecting a change in anticoagulation management in centers within ACTION.
- There were significantly fewer patients with a major bleed in the PSS group than in the BHS group, indicating improved anticoagulation management.
Future studies would benefit from randomizing bivalirudin use, quantifying the impact of being a part of a learning network, and casting a further net for data acquisition. Overall, the results support substantially improved outcomes, both survival and morbidity, for the post-approval study period. Ongoing collaboration will serve as an important component of continued improvement for pediatric VAD outcomes.
Featured researcher

Kathleen Simpson, MD
Pediatric cardiologist
The Heart Institute
Children's Hospital Colorado
Associate professor
Pediatrics-Cardiology
University of Colorado School of Medicine





 720-777-0123
720-777-0123










