Can modifications to a 120-year-old surgical technique solve complications and recurrence of pediatric rectal prolapse?
Rectal prolapse after repair of an anorectal malformation occurs at a frequency of 3.8% to 60%.
“Even when you do a perfect operation, the patient can have a rectal prolapse,” says Children’s Hospital Colorado pediatric colorectal surgeon Luis De La Torre, MD.
Although doctors don’t know why the large intestine slips outside of the anus in some patients, they suspect it might be due to insufficient innervation, weak attachment to the pelvis and underdeveloped muscle complex in the perineum. In other patients, it may happen when the rectum is very dilated. In addition to being aesthetically unpleasing, the condition produces outcomes such as bleeding, pain and ulceration.
There are several techniques to repair it. Some are very difficult to perform and can also lead to further complications or result in recurrences, says Dr. De La Torre.
Modifying a long-forgotten rectal prolapse technique
Dr. De La Torre is renowned for his revolutionary pull-through technique for Hirschsprung disease, called the De La Torre Technique, which combines what was originally three separate operations into one. The technique includes a transanal approach to complete a rectal mucosectomy, or the process of excising the mucous membrane from the rectum. During research on rectal mucosectomy for the De La Torre Technique, Dr. De La Torre found that there was a French surgeon in 1900 named Edmond Delorme who described a very similar technique for idiopathic rectal prolapse in elderly patients. No one seemed to be using that technique anymore, so Dr. De La Torre modified it with new sutures and began to use it for pediatric patients with idiopathic rectal prolapse.
“The results were great,” he says. “No recurrence, no reoperations. And I said, ‘Let’s try this in patients with imperforate anus.’”
Performing the technique
The technique dissects about 5 to 8 cm of rectal mucosa, exposing the muscle of the rectum. The team adds stiches on the rectum in a longitudinal way to create a plication or folds in the muscular wall, in all its circumference, forcing the proximal and distal mucosa closer to each other. They remove the dissected mucosa, shortening the muscle, and they connect the proximal and distal mucosa together with long-term absorbable sutures. It creates a unique and positive aesthetic effect and the anus appears closed.
“It’s a very easy solution to a very common problem,” says Dr. De La Torre.
Rectal prolapse repair
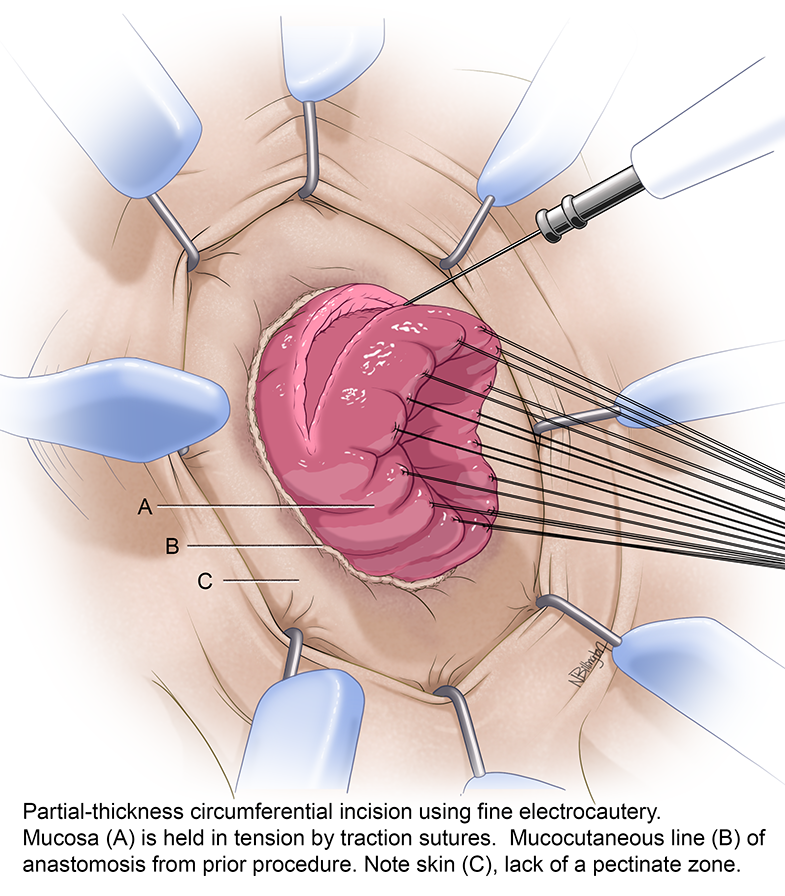
Partial thickness circumferential incision using fine electrocautery (A) Traction sutures are placed in the mucosa. (B) The mucocutaneous line from the previous anoplasty. (C) Skin: Note the lack of a pectinate line in the distal rectum.

Coronal view showing the longitudinal stitches in the muscular cuff (MC) Mucocutaneous line (A) Proximal mucosa (B) Distal mucosa
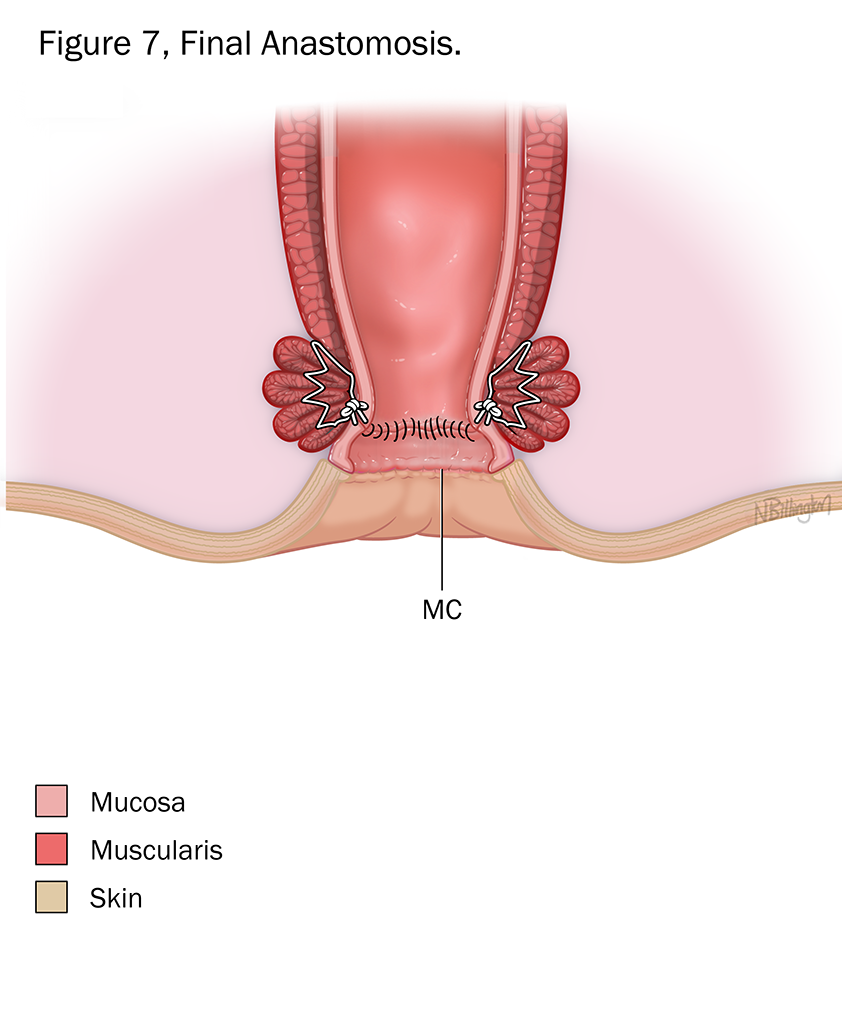
The mucosa was resected on the dotted line. The anastomosis (mucosa–mucosa) is completed. Note that the mucocutaneous line (MC) from the original anoplasty remains intact.
Featured Researchers

Luis De La Torre-Mondragon, MD
Pediatric colorectal surgeon
International Center for Colorectal and Urogenital Care
Children's Hospital Colorado
Associate professor
Surgery-Peds Surgery
University of Colorado School of Medicine





 720-777-0123
720-777-0123










