Key takeaways
-
Social determinants of health impact early prenatal detection of HLHS and TGA, both critical congenital heart defects requiring immediate postnatal specialized cardiac care.
-
Lower neighborhood socioeconomic quartile, rural residence and Hispanic ethnicity were the most significant factors identified.
-
Clinician education and a stronger link between affected populations, their obstetrical providers and tertiary care centers could improve health equity.
Statistics:
- <60% of congenital heart defects are diagnosed prenatally
- Two most common critical congenital heart defects are HLHS and TGA
- 85% of study participants were from the U.S. and the remainder were from Canada
Research background: prenatal detection of critical cardiac defects
Prenatal diagnosis can help reduce the morbidity and mortality of neonates with hypoplastic left heart syndrome (HLHS) and transposition of the great arteries (TGA), two of the most common critical congenital heart defects. However, less than 60% of these life-threatening cases are diagnosed prenatally.
By addressing gaps in medical literature and conducting more inclusive research studies, clinicians can better understand the barriers to receiving a prenatal cardiac diagnosis.
To the knowledge of the authors of this respective cohort study, it is the largest multicenter study identifying socioeconomic, race or ethnic, and geographic barriers to the prenatal detection of critical congenital heart disease in North America.
Researchers in this study sought to assess socioeconomic, demographic and geographic factors in the U.S. and Canada that affect rates of prenatal HLHS and TGA detection and postpone premature delivery of fetuses with cardiac defects.
Research methods: study population and variables
Participating centers were part of the Fetal Heart Society Research Collaborative and represented 21 medical centers across the U.S. and Canada, including the Colorado Fetal Care Center at Children’s Hospital Colorado. The study reviewed data between January 2012 and December 2016.
Patients included in the study were prenatally or postnatally diagnosed (before 2 months old) with HLHS or TGA with a recorded hospital visit. Inclusion criteria for HLHS and TGA were based on fetal or postnatal echocardiograms. Diagnosis was confirmed or made by postnatal echo or autopsy.
Study variables included:
- Neighborhood socioeconomic quartile (SEQ), a calculation of:
- Median household income
- Median housing value
- Percentage of high school graduates
- Percentage of college graduates
- Percentage of persons ≥16 years of age in executive, managerial or professional specialty occupations
- Percentage of households receiving interest, dividend or net rental income for each patient census tract
- Neighborhood poverty level >20%
- Race/ethnicity
- At-risk geographic location (United States–Mexico border, Native American reservation or island home) and rural residency (vs. urban, based on U.S. Department of Agriculture definition of categories 4 to 9)
- Distance from home to cardiac center of excellence and driving time
- Maternal insurance
- Maternal race or ethnicity
Research results: socioeconomic factors and prenatal diagnosis barriers
The study included 1,862 patients. Of those:
- 1,171 patients had HLHS (91.8% were prenatally diagnosed)
- 691 patients had TGA (58% were prenatally diagnosed)
- 1,582 patients (85%) were from the U.S.
- 280 (15%) patients were from Canada
- 133 had HLHS
- 147 had TGA
U.S. participant demographics:
- 43% had public insurance
- Race/ethnicity followed U.S. census trends
- 13% lived in a rural location
Socioeconomic factors associated with prenatal diagnosis

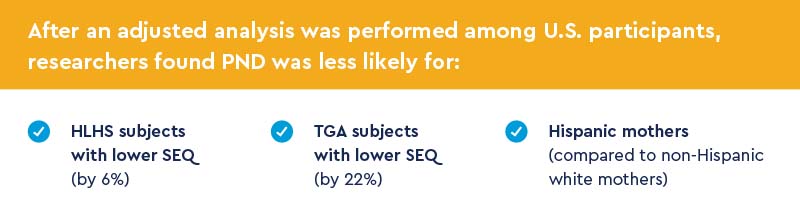
This was not true for Canadian participants except for among HLHS subjects living further from a care center.
Gestational age and PND associations
A lower SEQ was associated with a later gestational age at PND (after 24 weeks) for both conditions in the U.S. and Canada.
In the U.S.:
- Public insurance, rural residence and further distance of residence were associated with later gestational age at PND for both.
- Hispanic ethnicity was associated with later gestational age at HLHS diagnosis.
Research discussion: similar barriers faced by U.S. and Canada
Overall, while there are differences between the privatized healthcare system and Canada’s universal government programs, patients experienced similar barriers that impact their ability to access prenatal diagnosis. Access to more specific and personalized healthcare is a challenge for marginalized populations.
- For U.S. patients, lower SEQ was associated with lower PND of HLHS and TGA.
- For TGA, Hispanic ethnicity and rural location was also associated with decreased PND.
- For Canadian patients, only further driving distance to a cardiac center was associated with lower PND rates of HLHS.
Some barriers can be attributed to cardiac screening methodology. Many sites still evaluate only the four-chamber view of the heart, which will detect HLHS, but not TGA. Educating sonographers and obstetricians to include views of the aorta and pulmonary artery has been shown to improve detection of TGA.
Study authors noted differences between HLHS and TGA, suggesting that there may be barriers specific to the heart condition. But overall, mothers with a low SEQ were most disadvantaged in receiving a prompt prenatal diagnosis.
Research conclusions/clinical implication: clinicians’ role in reducing prenatal diagnosis barriers
Study authors wrote that the following could reduce disparities:
- Increasing clinician awareness and education about different socioeconomic factors that are barriers to prenatal diagnosis of TGA and HLHS
- Strengthening relationships between tertiary care surgical centers and primary care physicians
Featured Researchers
Bettina Cuneo, MD
Fetal cardiologist





 720-777-0123
720-777-0123










