What would it take to get kids and adults in the same study of an extremely rare type of kidney cancer?
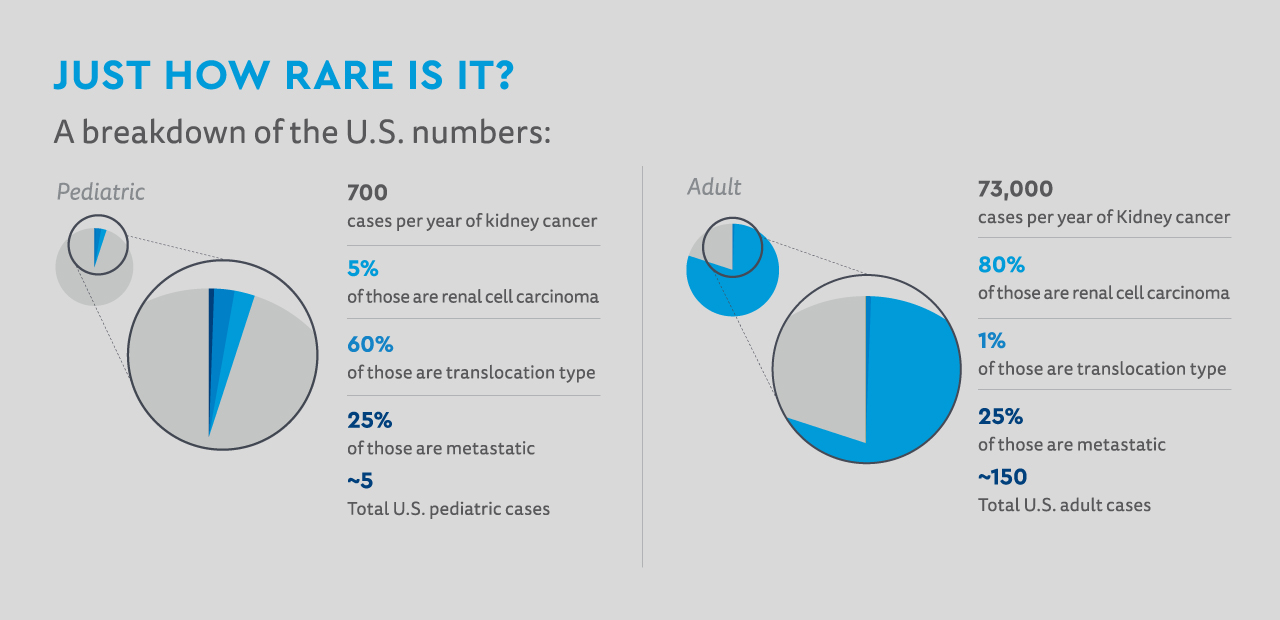
By any standard, translocation-type renal cell carcinoma, or RCC, is rare. It’s even rarer when it’s metastatic.
“People have said it’s so rare there’s no way to study it,” says Nick Cost, MD, one of just a handful of pediatric urologic oncologists in the nation.
But that difficulty doesn’t take away the need.
The difficulty of studying extremely rare cancers
RCC accounts for about 60% of pediatric RCC cases. On the adult side, that’s just 1% — but it’s still about 600 cases a year, as opposed to maybe 20 cases a year in kids. But for the 25% of those cases that metastasize, there’s essentially no treatment. Traditional chemotherapy is not effective.
Developing treatment would require data, but data was in short supply. Working with Cincinnati Children’s pediatric oncologist James I. Geller, MD, and the Children’s Oncology Group, the nation’s biggest pediatric cancer clinical trials consortium, Dr. Cost knew that even if they enrolled every case in the nation, it’d take several years.
“We decided to guide it not by age but by disease type,” says Dr. Cost.
Combining adult and pediatric cancer studies
On the adult side, the vast majority of RCC cases are clear cell-type, and two therapies have demonstrated effectiveness: nivolumab, an immune checkpoint inhibitor, and axitinib, a targeted inhibitor of a known growth pathway. There’s a good chance they’d work in translocation-type as well, but there’s no way to know without a trial.
And to do a trial they’d need adults. They’d have to convince their adult counterparts not only to commit time and resources to studying an extremely rare subtype of a rare disease, but to leave their comfort zone and enroll through an unfamiliar mechanism to do it.
Dr. Cost was undeterred. He and Dr. Geller went to adult oncology networks like the Eastern Cooperative Oncology Group, better known as ECOG, and the SWOG Cancer Research Network. They went to patient advocacy groups. They gathered data. They set up meetings.
“I’m a sucker for punishment,” Dr. Cost jokes. “It’s a lot of time and logistics and hours. But at the end of the day you go in there and you make such an airtight case this needs to be studied that the only way they can say no is if they just don’t like you.
“Just to get this study open,” he adds, “is a victory in itself.”
The road to treatment for metastatic translocation-type RCC
Even then, Dr. Cost expects to enroll about 18 patients per year. They’ll need three years to enroll and another three to follow the participants and see how they do. The hope, of course, is that the combination of therapies will be effective.
But even if they’re not, the study’s scaffolding — the partnerships and the mechanisms for enrollment and study it creates — sets the stage for many other studies like it. Studies of rare disease that affect pediatric and adult populations. Diseases never studied before.
“Where’s the threshold for too rare to study?” says Dr. Cost. “If it’s your child, who cares how rare it is? Rare should not be a deterrent. Rare is what we do.”
Featured Researchers

Nicholas Cost, MD
Co-director of Surgical Oncology
Department of Pediatric Urology
Children's Hospital Colorado
Associate professor
Surgery-Urology
University of Colorado School of Medicine





 720-777-0123
720-777-0123










