Key takeaways
-
Limited existing literature has shown neonates with end-stage renal disease often have poor outcomes after renal transplant.
-
A case series study of patients born with anuric end-stage renal disease who required renal replacement therapy within the first week of life found similar results.
-
Clinicians should give families an honest and nuanced assessment of the potential outcomes if they decide to proceed with prenatal amnioinfusion therapy.
Research background: Outcomes for patients with bilateral renal agenesis
Until recently, congenital bilateral renal agenesis (BRA) was considered a fatal diagnosis, primarily due to underdevelopment of the lungs resulting from low or absent amniotic fluid from lack of normal urine secretion by the fetus.
Amnioinfusion has made it possible for babies to survive until birth, but the procedure is controversial due to clinical and ethical concerns. Notably, these patients require dialysis almost immediately after delivery until they are eligible to receive a kidney transplant.
Prior study of outcomes after amnioinfusion looked at eligibility for kidney transplant and post-transplant survival rates for neonates with BRA.
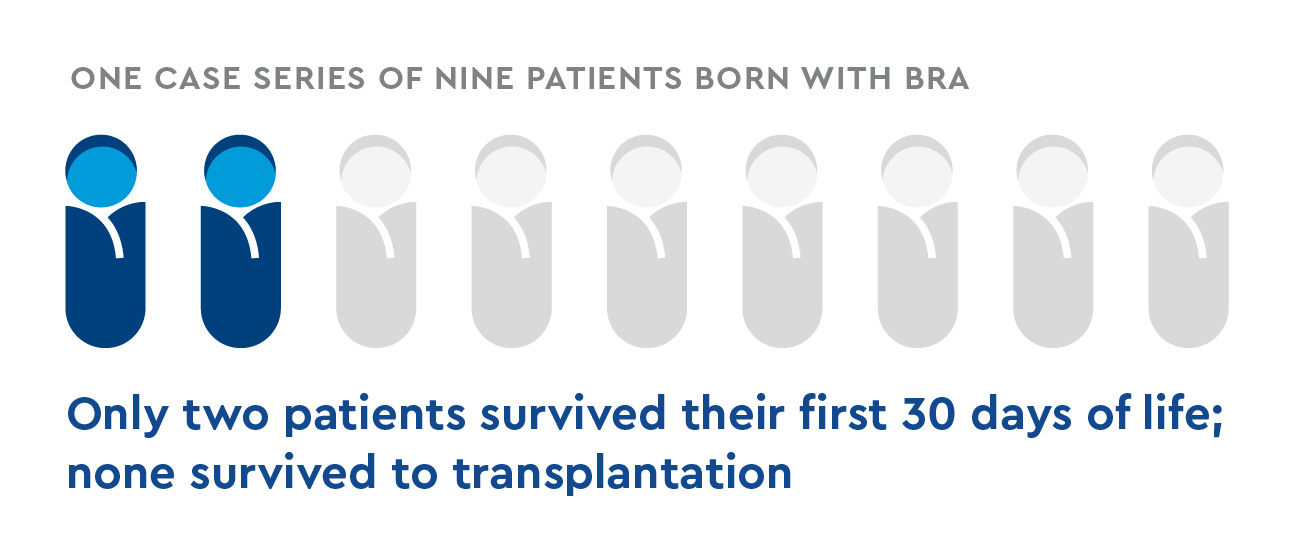
- Research focused on patients with bilateral renal agenesis is lacking.
- In one case series of nine patients born with BRA, only two survived their first 30 days of life; none survived to transplantation.
- Researchers sought to study patients with BRA and those born with end-stage kidney disease from other causes, focusing on patients who survived to eligibility for transplant and those who received a transplant. They also discuss the associated ethical implications of renal replacement therapy (RRT) in this population.
Methods: retrospective data collection
Pediatric urology and nephrology researchers from Children’s Hospital Colorado conducted a retrospective chart review of medical records and outcomes of Children’s Colorado patients born between 2009 to 2019.
Participant demographics
- BRA or anuric renal failure from other causes
- Received RRT within the first week of life:
- Peritoneal dialysis
- Continuous renal replacement type hemodialysis
- Hemodialysis via extracorporeal membrane oxygenation (ECMO)
Data collection
Outcomes measurement
- Number of patients who received a kidney transplant
- Survival at one year
- Overall survival
- Complications from RRT
- Peritonitis from peritoneal dialysis
- Other comorbidities
Results: Poor outcomes in patients born with end-stage renal failure
- Five patients met the criteria for inclusion in the case series study; four were female, one was male.
- RRT began at a median of three days after delivery.
- Four patients were alive one year after birth; three were alive at an average follow-up time of 39 months.
- Two were eventually able to receive a renal transplant, but only one was still living at follow-up.
- Four acquired comorbidities from dialysis, and two had significant complications:
- One had necrotizing enterocolitis from repeated failure of peritoneal dialysis and peritonitis, resulting in death.
- One had superior vena cava syndrome from prolonged intermittent hemodialysis, which made the patient ineligible for transplant.
Discussion: Poor outcomes make prenatal discussions challenging
Although the sample size was small, the researchers found that only 40% of patients were able to receive a renal transplant, and only half of those survived. Renal replacement therapy itself also led to frequent and significant complications, including patients becoming ineligible for transplant or even death. Caring for these infants also places intensive caregiving burdens on parents, which can place some families in economic hardship.
Prenatal discussions should include an accurate description of the likely postnatal outcomes, so that parents can make truly informed prenatal management decisions.
Conclusion: Healthcare providers must provide nuanced, realistic consultations
The study found success rates from renal transplantation are low in patients with BRA and similar conditions. When consulting parents about possible prenatal intervention, clinicians must include a nuanced discussion of the ultimate chances of success after birth, as well as infant and parental quality of life.
Featured Researchers

Margret Bock, MD
Pediatric nephrologist
Pediatric Nephrology
Children's Hospital Colorado
Associate professor
Pediatrics-Nephrology
University of Colorado School of Medicine
Jacqueline Glover, PhD
Center for Bioethics and Humanities
University of Colorado
Professor emerita
Pediatrics-Administration
University of Colorado School of Medicine

Vijaya Vemulakonda, MD
Pediatric urologist
Department of Pediatric Urology
Children's Hospital Colorado
Professor
Surgery-Urology
University of Colorado School of Medicine





 720-777-0123
720-777-0123










