- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Click to find the locations nearest youFind locations by region
See all locations -
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Colorado Hospitals Substance Exposed Newborn Quality Improvement Collaborative CHoSEN Conference (Hybrid)
Monday, April 29, 2024The CHoSEN Collaborative is an effort to increase consistency in...
-
Research & Innovation
- Overview
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.


Fetal Care Quality and Patient Safety
Advancing treatments to save lives and lifetimes.

Hearing that your baby has a prenatal (before birth) diagnosis that could affect their health can make you nervous. The best way to calm your nerves is to find a fetal center that can provide the best care for your baby and you. The Colorado Fetal Care Center at Children’s Hospital Colorado is that center.

Explore our outcomes
See all of our fetal care outcomes and learn more about the care we provide our families.
Quality and patient safety at the Colorado Fetal Care Center
Here, every provider involved in your baby’s care works toward one goal: the best possible outcome for you and your baby. That’s why we track and report our outcomes (success rates) and patient safety data. We want to know that we’re achieving the best results possible and that we have processes in place to constantly improve our care. We want you to know that, as well.
We compare our outcomes to national averages and other top fetal centers in the country. We share this information publicly so you have a clear view of our capabilities and the peace of mind that comes with it.
As one of the few truly comprehensive fetal care centers in the country, we treat virtually all fetal anomalies — even the very rare. And what’s even more important than the variety of conditions we treat is our rate of success.

“We believe in hope. That’s why we strive to give patients the best possible care for both mother and baby, from the very beginning.”Michael Zaretsky, MD
Why do outcomes and transparency matter?
Fetal anomalies are often serious conditions that require a specific level of experience and training. Families sometimes have to travel for the right care. If your child has a prenatal diagnosis, you want the best possible care for them. But it can be hard to know where to find that care. While many fetal centers track their outcomes, they don’t all report them publicly.
We believe that you should know our outcomes before you make decisions about your baby’s care. We’re proud of our outcomes and how they compare to other fetal centers, and we’re motivated to constantly improve them. We share them with you because we believe they will give you greater peace of mind when seeking care — and because it’s the right thing to do.
Our delivery and surgery volumes
A key measure of a successful fetal center is volume, which is the total number of surgeries, imaging tests, procedures and deliveries the center performs. Higher volume means providers have more experience performing certain procedures. Research shows that more experience correlates with better outcomes, such as higher survival rate and fewer complications.
This is particularly important for rare fetal anomalies. Having higher volumes indicates that we regularly treat patients with rare conditions that other fetal centers might only see once or twice a year.
As our volumes and outcomes show, the rare is common here.
Our delivery volumes
As one of just a few freestanding children’s hospitals in the country with a dedicated labor and delivery unit, Children’s Colorado offers a single, comfortable space where you can receive care before, during and after delivery. This is one of the many reasons so many parents with high-risk deliveries choose us.
What we measure:
We track our total deliveries and deliveries by condition. Only moms carrying a baby with a fetal condition deliver at our Center.
2,000+
Deliveries since 2012
2023 deliveries at a glance
What it means:
We have a level of expertise that only exists with a team that specializes in fetal care, and only fetal care. The babies and families we care for have complex conditions and they need a highly specialized and trained care team. Our volumes show that our care team is just that.
Our surgery volumes
We provide many surgical options from minimally invasive procedures to open fetal surgery.
What we measure:
Our total volume of surgeries for the life of our Center and type of surgery for the past year.
900+
Total surgeries performed (since 2012)
4
Fetal surgeons
1,200+
Surgical evaluations annually
2023 fetal surgeries at a glance
What it means:
Research shows that greater volumes lead to better outcomes. Our fetal surgeons and multidisciplinary team have experience and training in all fetal surgeries. If your baby needs surgery, before or after birth, you want one of the most experienced fetal surgical teams in the country, and you will find that at the Colorado Fetal Care Center.
Our fetal imaging test volumes
Our team of specially trained fetal radiologists, fetal cardiologists, fetal sonographers and maternal fetal medicine doctors provide fetal ultrasounds, fetal MRIs and fetal echocardiograms.
What we measure:
Our total number of fetal imaging tests, including ultrasounds, fetal MRIs and fetal echocardiograms we perform each year.
3,000+
Ultrasounds performed annually
300+
Fetal MRIs performed annually
1,800+
Fetal echocardiograms performed annually
What it means:
Our fetal imaging technologists, fetal radiologists and maternal fetal medicine doctors see thousands of images a year and focus only on prenatal (before birth) diagnoses. They have a trained eye that only experience can bring, which means you get the most accurate diagnosis.
Our twin-to-twin transfusion syndrome outcomes
Twin-to-twin transfusion syndrome (TTTS) is a serious and rare condition in identical twins who share a placenta. An imbalance in circulation of fluid and blood can create severe complications in twins. We treat the most severe and complex cases of TTTS that other fetal centers might not treat at all.
What we measure:
We track survival rates for one and both twins in TTTS pregnancies and our total selective fetoscopic laser photocoagulation (SFLP) procedures to repair TTTS. A number of factors impact survival, including severity of the condition, when it was diagnosed, risk of prematurity and the presence of selective fetal growth restriction.
64.9%
Survival for both twins since 2012 (higher than national benchmark)
411
SFLPs between 2012 and 2022
90.5%
Survival for at least one twin since 2012 (higher than national benchmark)
The following table shows our survival rates compared to the Solomon Group, an industry benchmark that we compare ourselves to. The Solomon Group was part of a clinical trial to establish expected outcomes for TTTS pregnancies that require SFLP, and advanced surgical treatment.
Twin-to-twin transfusion survival rates (Jan. 2012 to Dec. 2022)
| Solomon Group | Children's Colorado Group | |
|---|---|---|
| Overall survival | 74% | 76.2% |
| At least one surviving neonate | 85% | 87.4% |
| Double survival | 64% | 64.9% |
| TAPS or recurring TTTS | 4% | 4.1% |
What it means:
We perform a high volume of SFLPs and higher volumes lead to better outcomes. When compared to the Solomon Group, the Colorado Fetal Care Center has higher survival rates for one or both twins. We achieve these survival rates even though we treat the most severe cases of TTTS.
Learn more about our TTTS outcomes and care
Our myelomeningocele outcomes
Myelomeningocele (MMC) is a serious form of spina bifida, a birth defect of the spine and spinal cord. MMC occurs when the baby’s spine, spinal cord and spinal canal don’t close properly. We often treat MMC with open fetal surgery, which can reduce the need for a shunt and improve movement for your baby.
What we measure:
We measure the shunt rate, which is how often a baby with MMC will need a shunt at some point to help drain excess spinal fluid from the brain. A shunt increases the chances for further complications in the future, so the lower the rate the better. We compare our shunt rate to a national study (MOMS), in which the benchmark is 40%.
Our team also reports the total MMC surgeries we've performed since 2012.
38%
Shunt rate since 2012 (lower than national benchmark)
108
MMC surgeries since 2012
What it means:
When compared to the outcomes of a national study on surgical repair of MMC, we have a a lower shunt rate thanks to our experienced team and multidisciplinary approach. This reduces the risk for future complications and means the baby doesn’t need a shunt placement operation.
Our total volume of surgeries illustrates that we have one of the most experienced surgery teams in the country for MMC repair. Higher volumes lead to better outcomes for babies and families with MMC.
Learn more about our MMC outcomes and care
Our congenital diaphragmatic hernia outcomes
Congenital diaphragmatic hernia (CDH) is a birth defect that occurs when a baby’s diaphragm doesn’t form correctly creating an opening between the chest and abdominal cavities. This allows abdominal organs to enter the chest cavity and prevent lung development.
We treat CDH both before and after birth depending on what is best for each baby.
What we measure:
We measure overall volume of patients with CDH, survival rate and percentage of patients who deliver their babies at Children’s Colorado when clinically necessary.
216+
Patients with CDH treated since 2012
79%
CDH survival since 2012
What it means:
At the Colorado Fetal Care Center and our Neonatal Intensive Care Unit, we have some of the highest volumes and one of the highest survival rates for CDH in the country. We’re also helping more moms deliver at their home hospital when possible by providing care before birth and working closely with their primary doctors. We are delivering some of the best results for the most severe CDH cases and limiting disruption for families with less severe cases.
This data is collected by the Department of Epidemiology at Children's Colorado using information provided to them by the Colorado Fetal Care Center and NICU. We update this information on an annual basis.
Our fetal cardiology volumes and outcomes
At the Colorado Fetal Care Center, our renowned Fetal Cardiology Program cares for babies with a wide range of heart problems, including congenital heart defects (CHDs), cardiomyopathies and arrhythmias. Heart conditions represent the largest percentage of our deliveries in the Colorado Fetal Care Center.
When a structural or heart rhythm problem is detected prenatally, our fetal care team provides an accurate diagnosis and an individualized care plan just for your baby. Treating certain heart conditions before birth can improve long-term outcomes. As soon as your baby is born, colleagues in our nationally-ranked Heart Institute are equipped to provide all the care your baby may need, from surgery to cardiac catheterization to device placement and beyond.
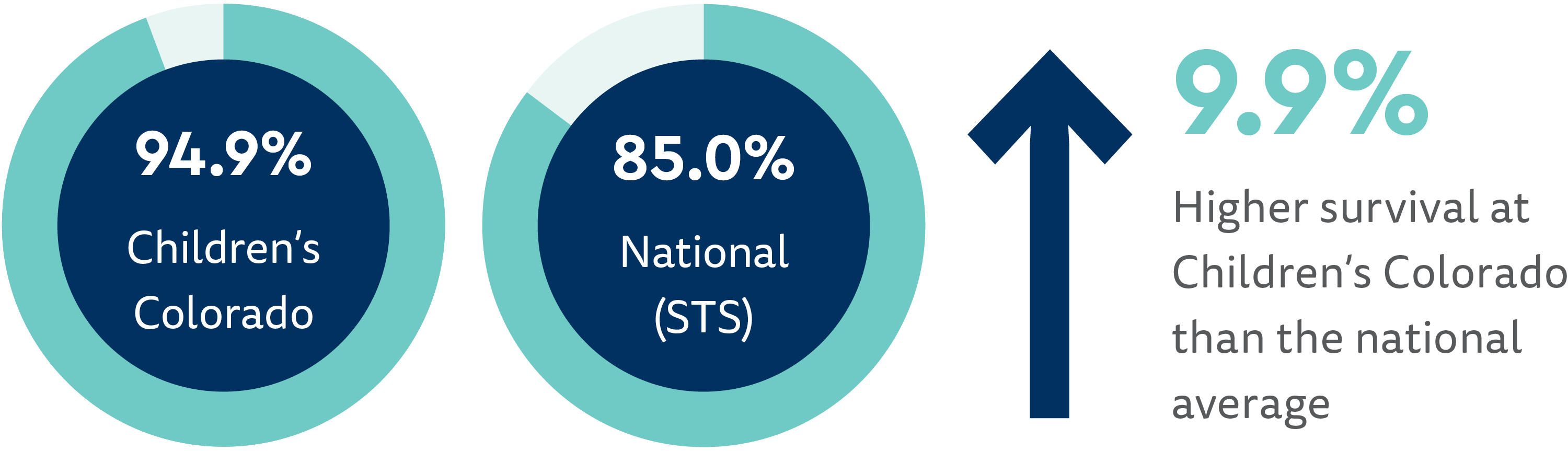
When it comes to the most risky and complex heart surgeries, known as a STAT 5 surgery, our fetal cardiology program out-performs the national average.
See our Heart Institute’s full volumes and exceptional outcomes in cardiac surgery, heart transplantation and overall quality and patient safety.
Learn more about our fetal cardiology outcomes and care
Patient experience at the Colorado Fetal Care Center
Our goal is to provide excellent care to babies and their families throughout their stay. We measure that through patient experience surveys with our families. For 2023, families rated their experience on a scale of 0 to 10, with 10 being the best experience. We receive feedback on our inpatient experience, which is our high-risk pregnancy labor and deliver unity, and our outpatient experience, which is when we see moms for consultations, imaging tests and other services.
91%
Of patients rated their inpatient, labor and delivery, experience as a 9 or 10
97%
Of patients rated their outpatient experience as a 9 or 10
We track patient and family experience by surveying families over the phone and through email. This measure is based on how each patient or family answers the following questions:
- "Using any number from 0 to 10, where 0 is the worst facility possible and 10 is the best facility possible, what number would you use to rate this facility?" and
- "Using any number from 0 to 10, where 0 is the worst provider possible and 10 is the best provider possible, what number would you use to rate this provider?"
We then report the percentage of families who rated us as a 9 or a 10 on the scale.
A third-party company conducts these surveys on our behalf, and then compiles the patient experience data for our hospital and departments. Learn about how we measure overall patient experience at Children’s Colorado.

Would you like a second opinion?
If you have received a prenatal diagnosis, are considering treatment options or just want to feel more confident about your treatment plan, our fetal care experts are here to help.
Request a second opinion from our Colorado Fetal Care Center
Additional resources
We measure our outcomes on a continual basis to ensure we’re providing the best possible care while meeting or exceeding the high standards we set for ourselves. We are committed to sharing those outcomes with you and providing any additional helpful information. Visit the resources below to learn even more.
- Learn how to plan for your visit to the Colorado Fetal Care Center.
- Read frequently asked questions about the Colorado Fetal Care Center.
- Learn more about our nationally-ranked Heart Institute.
- The Fetal Health Foundation provides a wealth of resources for families with a prenatal diagnosis.
Learn more about choosing a fetal care center:



 720-777-0123
720-777-0123




