- Doctors & Departments
-
Conditions & Advice
- Overview
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
- Baby Guide
-
Your Visit
- Overview
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Click to find the locations nearest youFind locations by region
See all locations -
Community
- Overview
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
Upcoming Events
Colorado Hospitals Substance Exposed Newborn Quality Improvement Collaborative CHoSEN Conference (Hybrid)
Monday, April 29, 2024The CHoSEN Collaborative is an effort to increase consistency in...
-
Research & Innovation
- Overview
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health.


Intrauterine Device (IUD)
We’re passionate about providing answers, treatment and care for the full range of female reproductive health concerns, from infancy through adolescence and into adulthood.
What is an intrauterine device (IUD)?
An intrauterine device, or IUD, is a type of birth control that’s inserted into the uterus to prevent pregnancy. Because IUDs also release hormones, we can use them for hormonal therapy to manage periods, including menstrual suppression. Menstrual suppression helps lessen the effects of periods such as pain and bleeding. In pediatric and adolescent gynecology, we use a hormonal IUD to treat heavy periods, painful periods, endometriosis and many other conditions.
The IUD is also a long-acting contraceptive device that’s highly effective at preventing pregnancy. The IUD brands Mirena® and LILETTA® are currently FDA-approved for 8 years. At that time, your doctor can replace the IUD with a new one, if desired. We can also remove the IUD sooner than 8 years, if requested.
Learn more about getting an IUD to help with periods:
Learn more about myths and facts about IUDs:
How does an IUD work?
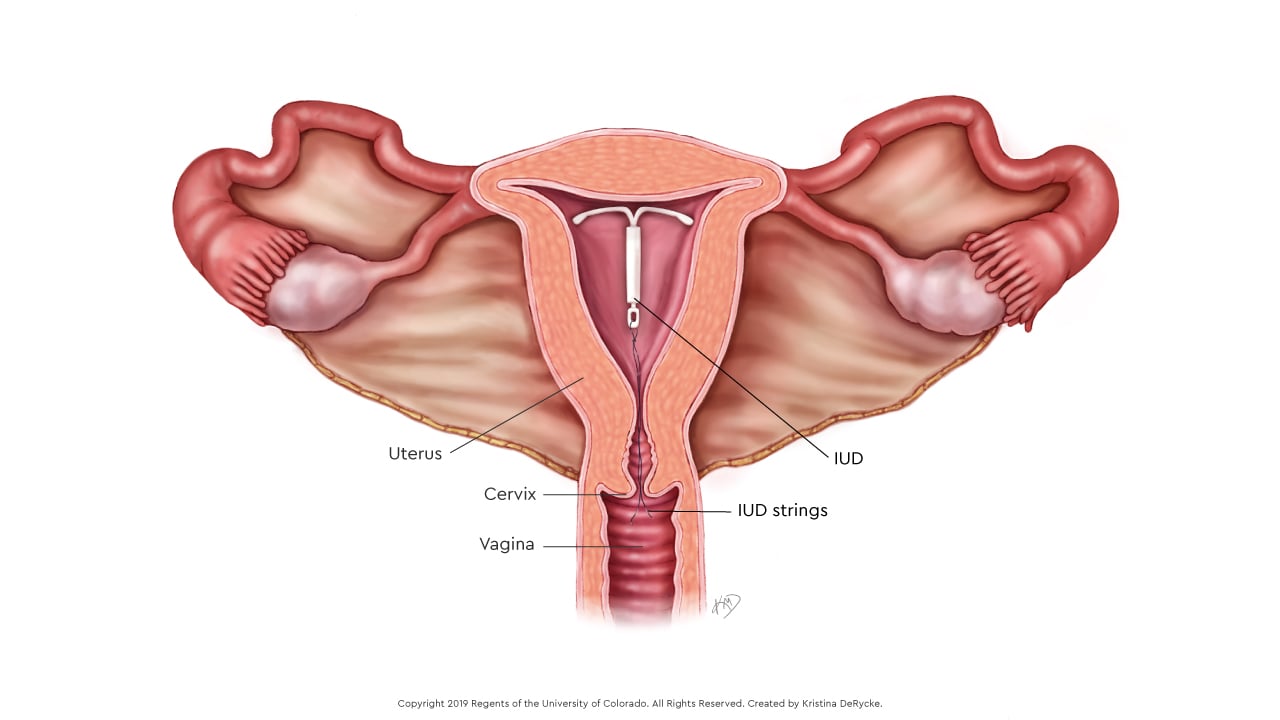
The IUD sits inside the uterus and releases a medication called progesterone.
Progesterone thins the lining of the uterus so menstrual periods are very light or don’t occur at all. In addition to reducing blood loss from periods that cause heavy bleeding, we can also use IUDs to treat endometriosis and reduce pelvic pain and cramping.
The IUD works as birth control because it blocks sperm from reaching the fallopian tubes where fertilization occurs. Most people who have an IUD will have less bleeding over time. If periods suddenly become heavy and regular again, please let us know.
How to prepare for an IUD placement procedure
The IUD is a safe and effective way to reduce or stop menstrual periods, cramping and bleeding. If you’re a parent bringing your child in for the procedure, reassure them it’s safe and they will not feel the IUD inside their uterus afterwards. You or your child can also enjoy all the same activities as before the procedure.
Before the appointment, we recommend you have ibuprofen (Motrin), acetaminophen (Tylenol), menstrual products and a heating pad at your house for when you return.
On the day of the appointment:
- Eat and drink normally.
- Take ibuprofen about 30 minutes before your visit.
- Arrive 15 minutes early for check-in.
- Be sure you can give a urine sample at the start of your visit.
IUD placement without anesthesia (in the clinic)
We can place the IUD during an office visit without any anesthesia. For this method, we suggest patients take a mild, over-the-counter pain reliever 30 minutes before the appointment.
IUD placement with intranasal midazolam (Versed®) (in the clinic)
We can also place the IUD accompanied with intranasal (through their nose) medication. Midazolam is the generic name for Versed®, which is a medication we use before procedures to help with anxiety and provide mild sedation. You or your child will inhale the medication through the nose 10 minutes before the start of the procedure. Common side effects might include nasal irritation and headaches.
What to expect during an IUD placement with intranasal midazolam
You or your child will be awake for the duration of the procedure. The IUD insertion itself takes between 5 and 15 minutes with some additional time before and after. We’ll ensure you or your child’s vital signs are normal before allowing you to leave the hospital. You will need someone to accompany you and drive you home after the procedure.
What to expect after an IUD placement with intranasal midazolam
You or your child will be able to go home shortly after the procedure. We recommend not driving for the remainder of the day. Patients may return to school or work after the procedure if they feel up to it, but we recommend taking the rest of the day off after the procedure.
Patients can use over-the-counter medication for pain if they need it at home. Some may experience light menstrual bleeding or spotting following the procedure, but others will have no bleeding at all. If you or your child experience cramping, use a heating pad to ease the discomfort, as well as medication commonly used for menstrual cramps such as ibuprofen.
During the first 3 to 6 months of using the IUD, there may be irregular bleeding or spotting (light bleeding or brownish discharge). This may happen every day or only a few days per month. Over time, menstrual periods are usually very light or do not occur at all.
Please call our nursing line at 720-777-2667 if cramping continues longer than one week after getting an IUD, or if you have fever, chills, severe pain, cramping, or increased or heavy bleeding.
IUD placement with anesthesia (in the procedure center)
Some prefer to have anesthesia for the IUD placement procedure. Our doctors suggest an IUD insertion under anesthesia if your child can’t tolerate a pelvic exam or the pain caused by the insertion procedure. Other common reasons for placing IUDs under anesthesia include:
- Teens and young adults with development delays and special medical needs may request menstrual suppression
- Previous attempts at insertion without anesthesia have been unsuccessful
- Those with chronic pelvic pain or endometriosis may not be able to tolerate an IUD insertion without anesthesia
What to expect during an IUD placement under anesthesia
After the anesthesiologist gives the anesthesia and the patient is asleep, the doctor performs a gentle pelvic exam to understand the direction and size of the uterus. They then place a small instrument, called a speculum, inside the vagina so they can see the cervix, which is the opening to the uterus. The doctor measures the uterus in length, places the IUD inside, then cuts the string of the IUD so they can easily remove it later.
It usually takes less than five minutes to insert the IUD, however, most patients spend about 3 to 4 hours at the hospital for an IUD insertion under anesthesia. This total time includes preparing for the procedure, medication for anesthesia and waiting for the anesthesia to wear off after the procedure. We invite families to stay with their children before and after the procedure.
What to expect after an IUD placement under anesthesia
With minor procedures like this, patients usually wake up in the postoperative area hungry and eager to go home. You or your child can eat and drink in the post-op area as soon as they wake up and can leave once the doctor says they can go home.
Most patients who receive general anesthesia have no cramps or pain for the first 24 to 28 hours after the procedure due to the anesthesia medication. Patients can use over-the-counter medication for pain if they need it at home. Some may experience light menstrual bleeding or spotting following the procedure, but others will have no bleeding at all. If you or your child experience cramping, use a heating pad to ease the discomfort, as well as medication commonly used for menstrual cramps such as ibuprofen.
Plan on having a relaxed day after getting an IUD. We recommend that you or your child do not drive or operate any heavy machinery for the remainder of the day. While some may feel like they can go to work or school, we recommend going home to rest. Most patients can return to normal activities the day after their procedure.
During the first 3 to 6 months of using the IUD, there may be irregular bleeding or spotting (light bleeding or brownish discharge). This may happen every day or only a few days per month. Over time, menstrual periods are usually very light or do not occur at all.
Please call our nursing line at 720-777-2667 if cramping continues longer than one week after getting an IUD, or if you have fever, chills, severe pain, cramping, or increased or heavy bleeding.
Why choose us for an IUD placement?
Our doctors at Children’s Colorado have decades of experience using the hormonal IUD for menstrual suppression and treating other gynecologic conditions as well. In addition to their extensive experience with IUDs, all our doctors and nurses are trained to work with children and teens and are skilled at helping put them and their families at ease before, during and after the procedure. While some hospitals may not have pediatric-trained anesthesiologists, ours are specially trained to work with children and teens, as well as with adults.
If you have any questions or concerns, call the ParentSmart Healthline toll free at 1-855-KID-INFO (543-4636). Caring pediatric nurses are available 24 hours a day, 7 days a week to help.
We have many safe options for people who don’t want to have regular menstrual periods. For teens with special needs or medical conditions, menstrual hygiene can be difficult. Also, periods can make other issues like headaches, mood changes and seizures worse.
Many teens and their families decide to have a progestin IUD to stop or reduce menstrual bleeding. Some reasons why they may choose an IUD over other options include:
- The IUD is very safe. The medicine in the IUD is only released inside the uterus. For teens with complex medical issues, especially blood and heart problems, the IUD doesn’t interfere with other medications or affect other body systems.
- The Mirena® and LILETTA® IUDs works for eight years on its own. After eight years, we can remove and replace the IUD.
- Some people can’t or don’t like to swallow pills. The IUD works without having to remember to take a pill each day.
- The IUD reduces or eliminates pelvic pain and cramps.
- The IUD is an excellent type of birth control. Even if this isn’t the main reason for getting an IUD, teens and families may want an option that prevents pregnancy.
- We can place the IUD under anesthesia. This means that someone will be asleep during the pelvic exam and placement procedure. Once placed inside the uterus, a person can’t tell that they have an IUD.
| Brand name | Length of effectiveness | What's in it? | Effect on periods |
|---|---|---|---|
|
Mirena® |
8 years |
Progestin |
Lighter and less painful periods |
|
LILETTA® |
8 years |
Progestin |
Best chance of no period at all |
|
Kyleena® |
5 years |
Progestin |
Likely to have lighter periods |
|
Skyla® |
3 years |
Progestin |
Likely to have lighter periods |
|
Paraguard |
12 years |
Non-hormonal, copper IUD |
Likely that periods will be heavier and more painful We do not recommend if you have bad cramps or heavier menstrual flow as it will make it worse. |
Here are some answers to some frequently asked questions that our teen and young adult patients ask us about Intrauterine Devices (IUDs). If you have any additional questions, please feel free to call us at 720-777-2667.
Is it really safe not to have a period?
Yes. Not having a period (or only really light bleeding) is one of the best parts about having a progestin IUD. The medicine in the IUD prevents the lining of the uterus from getting thick. This means that it’s safe to not have periods.
How long does it take to place the IUD?
The actual pelvic exam and IUD placement takes less than 5 minutes. If you’re not getting anesthesia, your appointment will be scheduled for about 30 minutes or more because you need to give a urine sample, talk to the nurse and doctor about your health history and get ready for the procedure.
How will the progestin IUD affect my acne?
If you have moderate or severe acne, the progestin IUD may make it a bit worse. But there are many medications that you can use to make it better. The birth control pill, patch and ring can help make acne better. If you’re switching from one of these methods to an IUD and have had bad acne in the past, talk to your doctor about what to expect with using the IUD.
Is it safe to take another hormonal therapy and use an IUD?
Yes. Sometimes people need to use two different methods to help with their periods or other concerns. This is safe if prescribed by your doctor.
Can I still use a menstrual cup when I have an IUD?
The menstrual cup is a great option for dealing with period blood, but there have been some infrequent reports of people accidentally pulling out their own IUD with use of the cup. Talk to your doctor if you are planning to use a menstrual cup while using an IUD. Tampons are always safe to use when you have an IUD.
Why am I still bleeding with my progestin IUD?
Some people have frequent bleeding and spotting for the first 3 to 6 months after getting a progestin IUD, and sometimes even longer. Please let your doctor know if this is bothering you as they may want to perform tests or prescribe medications that will help it go away.
My partner said they can feel my IUD strings. What does this mean?
There are strings attached to the IUD that come out at the opening of the cervix. This is at the very end of the vagina and usually a partner can’t feel them because they get curled up and tucked away. If your partner can feel the strings but they do not bother them in any way, this is OK, and you don’t need to do anything. If the strings are bothersome or seem to have changed in some way, please call your doctor and let them know.
What is the best type of IUD?
We most often recommend the Mirena® or LILETTA® IUDs because they are the best at treating menstrual problems as well as being great birth control.
What is the medicine inside the IUD?
The medicine in the IUD is called levonorgestrel. This is a type of progestin, which is a synthetic version of the hormone progesterone, naturally made by the body at the time of ovulation. Levonorgestrel has been studied for many decades and all the scientific evidence shows that it’s safe to use, even for long periods of time.
What causes the brown discharge that I have with my IUD?
Sometimes people with a progestin IUD will notice brown or yellowish discharge that might look like mucus or old blood. Check in with your doctor to make sure you don’t need tests, but usually this is a normal side effect of the IUD. It happens because the IUD thins out the lining of the uterus so there isa tiny amount of bleeding (spotting) that then turns brown or even black as it gets older. The progestin in the IUD also thickens cervical mucus, which may change the type of vaginal discharge while using an IUD.



 720-777-0123
720-777-0123